Cholesterol is essential to our cell membranes, hormones, and bile acids. However, high cholesterol levels in the blood can increase the risk of heart disease and stroke. Therefore, understanding the complex process of cholesterol synthesis and regulation in our body is crucial for maintaining our health.
This article will explain the step-by-step mechanism of cholesterol synthesis, its key enzymes and genes, and the feedback mechanisms that control its production and transport.
What is Cholesterol?
Cholesterol is a sterol, a type of lipid molecule composed of a complex structure of four fused hydrocarbon rings.
- The chemical formula of cholesterol is C27H46O, and its molecular weight is 386.66 g/mol.
- Cholesterol is a hydrophobic molecule that is insoluble in water and nonpolar solvents, such as ether, chloroform, and benzene.
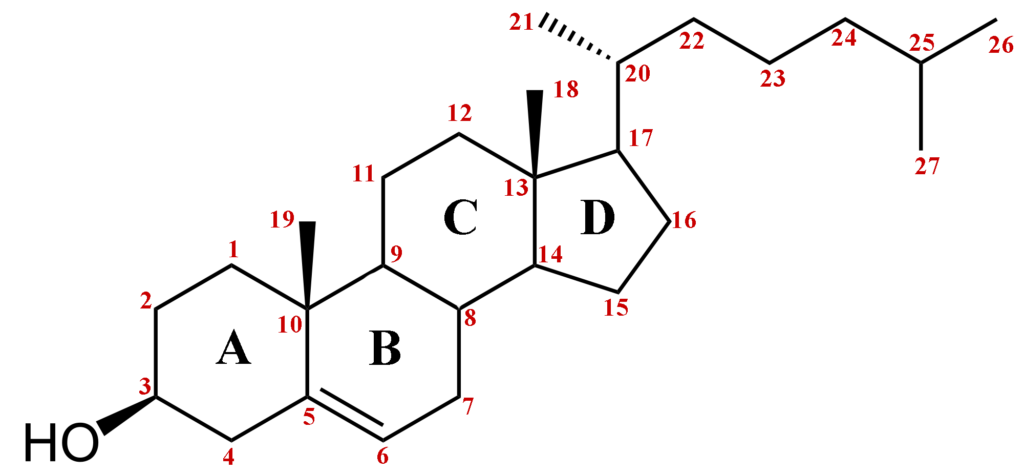
The structure of cholesterol is composed of three central regions:
- A hydrophilic hydroxyl group (-OH) at position 3.
- A hydrophobic hydrocarbon tail at position 17.
- A steroid nucleus that contains four fused rings.
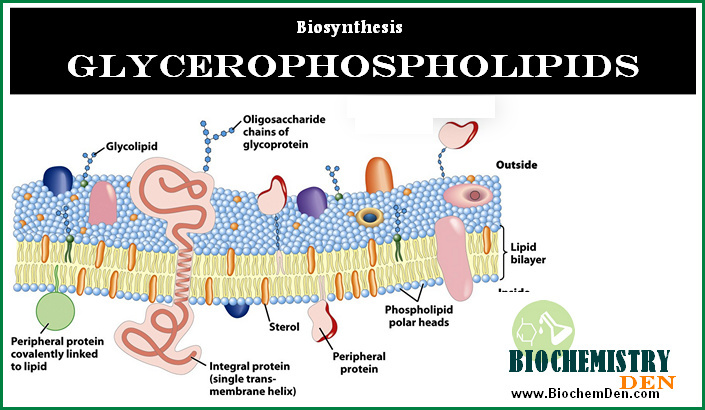
The hydrophilic hydroxyl group enables cholesterol to form hydrogen bonds with water molecules. At the same time, the hydrophobic tail allows it to associate with other lipids and form stable lipid bilayers in cell membranes.
- The steroid nucleus of cholesterol consists of four rings labeled A, B, C, and D.
- Rings A, B, and C are cyclohexane rings, while ring D is a cyclopentane ring.
- The rings are labeled with numbers and letters to identify the positions of the various functional groups that are attached to the rings.
The orientation and arrangement of the rings and functional groups determine cholesterol’s unique properties and functions.
Cholesterol is a precursor molecule for synthesizing several essential compounds in the body, including steroid hormones, bile acids, and vitamin D.
In addition, cholesterol plays a critical role in maintaining cell membranes’ structural integrity and fluidity. Cholesterol interacts with other lipids, such as phospholipids, to form lipid bilayers essential for cell membranes‘ function.
The Pathway of Cholesterol Synthesis
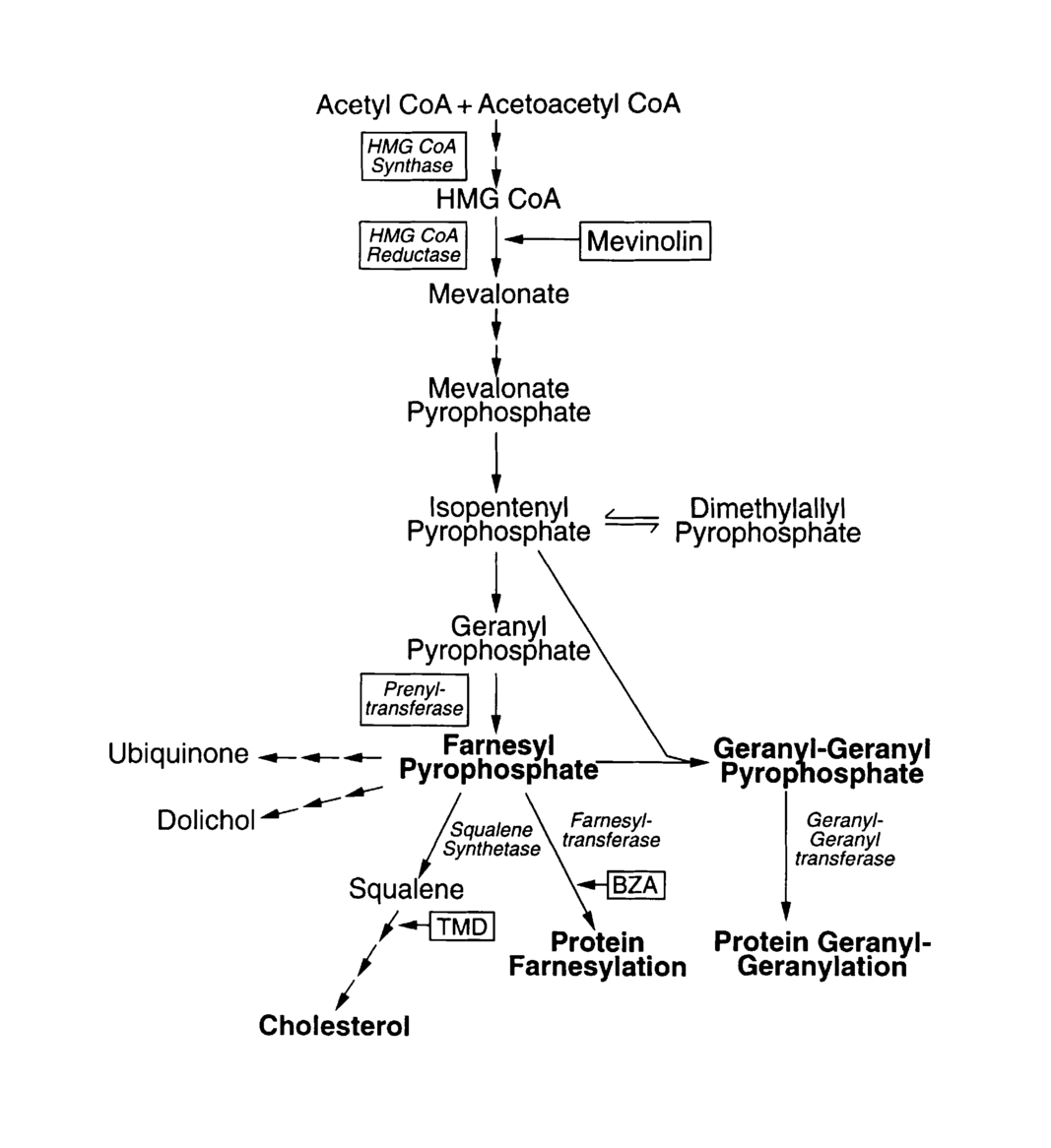
Cholesterol synthesis occurs mainly in the liver and other tissues, such as the intestine and adrenal glands. The first and rate-limiting step of cholesterol synthesis is the conversion of acetyl-CoA to mevalonate by the enzyme HMG-CoA reductase (HMGCR).
Mevalonate then undergoes a series of enzymatic reactions to form isoprenoids, precursors of cholesterol.
Cholesterol synthesis is a complex process involving a series of enzymatic reactions and regulatory steps in various cell organelles. Here are the detailed steps of the cholesterol synthesis pathway:
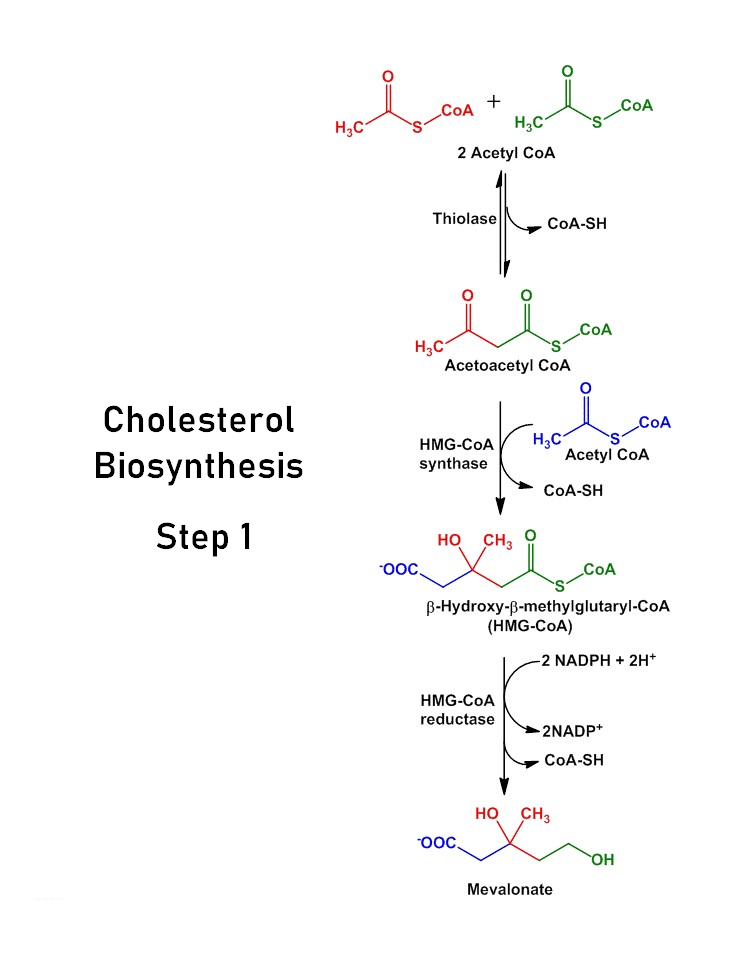
Step 1: Acetyl-CoA to HMG-CoA
- Cholesterol synthesis starts in the cell’s cytosol with the conversion of two molecules of acetyl-CoA into a four-carbon molecule called acetoacetyl-CoA, which is then converted into 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) by the enzyme HMG-CoA synthase.
- This reaction is the committed step of cholesterol synthesis and is regulated by feedback inhibition by cholesterol and its derivatives.
- The chemical equation for this reaction is:
2 Acetyl-CoA + ATP + H2O → HMG-CoA + CoA + ADP + Pi
Step 2: HMG-CoA to Mevalonate
- The next step of cholesterol synthesis occurs in the endoplasmic reticulum (ER), where HMG-CoA is converted into mevalonate by the enzyme HMG-CoA reductase (HMGCR).
- It is a rate-limiting step of cholesterol synthesis and is also subject to feedback regulation by cholesterol and its derivatives.
- The chemical equation for this reaction is:
HMG~CoA + 2 NADPH + 2 H+ → Mevalonate + 2 NADP+ + CoA
Step 3: Mevalonate to Isoprene Units
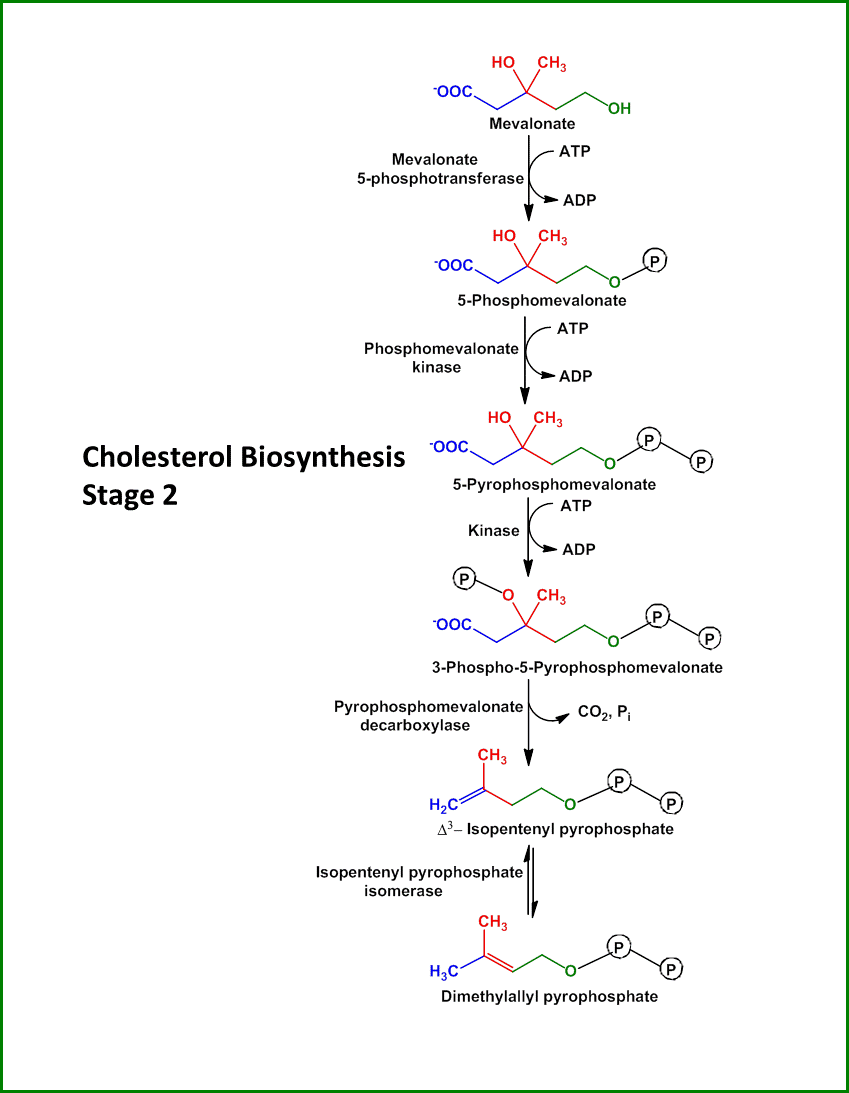
- Mevalonate is then converted into five-carbon isoprene units by a series of enzymatic reactions, starting with the phosphorylation of mevalonate into mevalonate-5-phosphate by mevalonate kinase.
- The following steps involve the conversion of mevalonate-5-phosphate into 3-isopentenyl pyrophosphate (IPP) and its isomer dimethylallyl pyrophosphate (DMAPP) by the enzymes phosphomevalonate kinase, mevalonate pyrophosphate decarboxylase, and isopentenyl pyrophosphate isomerase.
- These isoprene units are the building blocks for cholesterol and other isoprenoids. The chemical equations for these reactions are:
Mevalonate + ATP → Mevalonate-5-phosphate + ADP
Mevalonate-5-phosphate → IPP + CO2
IPP ↔ DMAPP
Step 4: Isoprene Units to Squalene
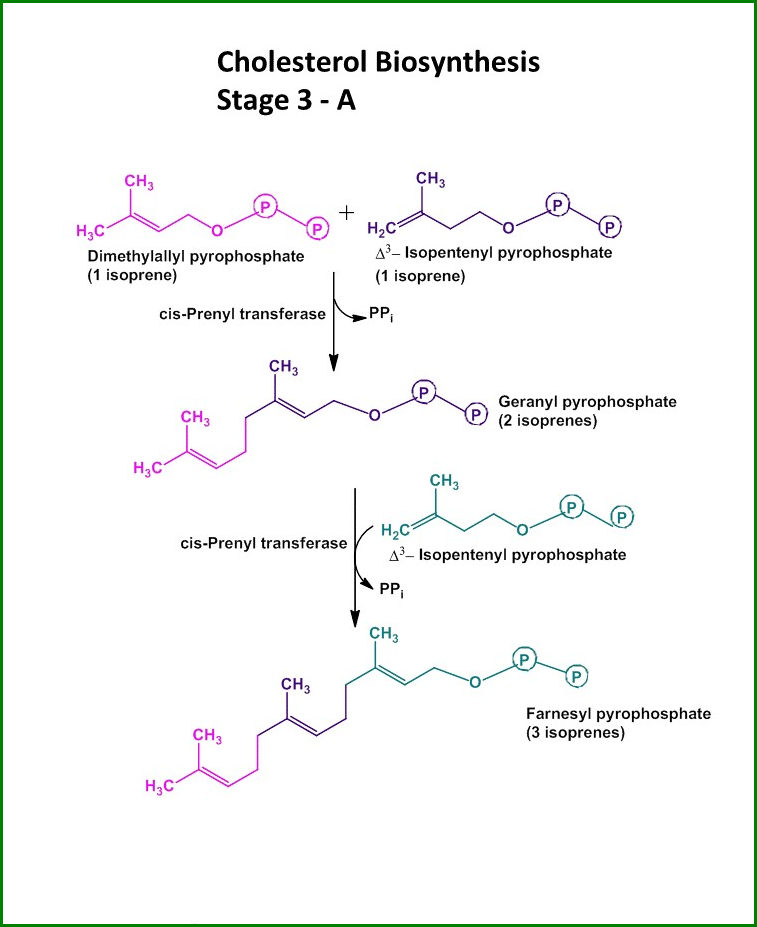
- The next step of cholesterol synthesis involves condensing six isoprene units (three IPP and three DMAPP) to form a 30-carbon molecule called squalene, which is catalyzed by the enzyme squalene synthase.
- The chemical equation for this reaction is:
6 IPP + 6 DMAPP → Squalene + 2 PPi
Step 5: Squalene to Cholesterol
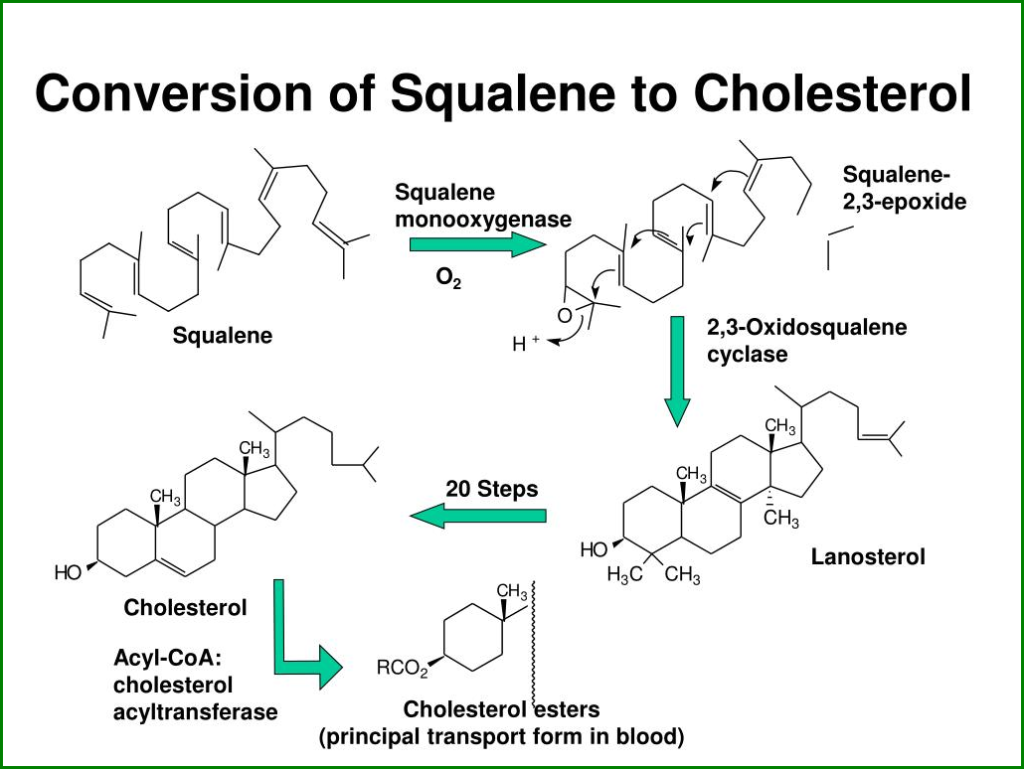
- Squalene is then converted into cholesterol through a series of enzymatic reactions involving the cyclization and rearrangement of squalene into lanosterol and its subsequent modification and cleavage into cholesterol.
- These reactions occur in the ER and involve the enzymes lanosterol synthase, 14-alpha-demethylase, and several other enzymes.
- The chemical equations for these reactions are complex and involve multiple steps, but the overall process can be summarized as follows:
Squalene → Lanosterol → Cholesterol
Cholesterol synthesis is a complex process involving multiple enzymatic reactions and regulatory steps in different cell organelles.
Understanding the detailed steps of the cholesterol synthesis pathway is crucial for developing new therapies for related disorders and improving our knowledge of cholesterol metabolism.
The Regulation of Cholesterol Synthesis
Cholesterol synthesis is not a constant process but a tightly regulated one. The feedback mechanisms that control cholesterol synthesis involve several transcription factors, membrane receptors, and signaling pathways.
The major players and their functions are:
a. Sterol regulatory element-binding proteins (SREBPs)
- SREBPs are transcription factors that activate the genes involved in cholesterol and fatty acid synthesis in response to low cholesterol levels in the cell membrane.
- SREBPs are synthesized as inactive precursors in the endoplasmic reticulum (ER) and processed by site-1 and site-2 proteases to release their active forms, which translocate to the nucleus and bind to the promoters of target genes.
b. Low-density lipoprotein receptors (LDLRs)
LDLRs are membrane receptors that internalize cholesterol-carrying LDL particles into the cells. When the intracellular cholesterol level is high, the expression of LDLRs is downregulated by a negative feedback loop that involves SREBPs and their target genes.
c. Liver X receptors (LXRs)
- LXRs are nuclear receptors that activate the genes involved in cholesterol efflux and reverse transport from the peripheral tissues to the liver for excretion.
- Oxysterols, oxidized cholesterol derivatives, start LXRs and form heterodimers with retinoid X receptors (RXRs) to bind to the promoters of target genes.
The Clinical Implications of Cholesterol Synthesis
Cholesterol synthesis and regulation are crucial for our normal physiology and relevant to several diseases and drugs. Some of the clinical implications of cholesterol synthesis are:
Hypercholesterolemia
- Hypercholesterolemia is characterized by high levels of total cholesterol in the blood, mainly due to high LDL cholesterol levels.
- Hypercholesterolemia can be caused by genetic mutations in the genes encoding for LDL receptors, apolipoprotein B, or PCSK9, which are involved in LDL metabolism, or by lifestyle factors such as a high-fat diet, obesity, and physical inactivity.
- Hypercholesterolemia is a significant risk factor for atherosclerosis, coronary heart disease, and stroke and is often treated with statins, which inhibit HMGCR and reduce cholesterol synthesis in the liver.
Hypocholesterolemia
- Hypocholesterolemia is a condition characterized by low levels of total cholesterol in the blood, which can be due to genetic mutations in the genes encoding for HMGCR, SREBPs, or other enzymes and transporters involved in cholesterol synthesis and regulation.
- Malabsorption syndromes, liver or kidney diseases, and some drugs such as cholestyramine and ezetimibe can also cause hypocholesterolemia.
- Hypocholesterolemia may protect against some conditions, such as Alzheimer’s and Parkinson’s, but may also increase the risk of infections and cancers.
Cholesterol-lowering drugs
- Several drugs are available to lower cholesterol levels in the blood, either by inhibiting cholesterol synthesis, such as statins or by increasing cholesterol excretion, such as bile acid sequestrants and PCSK9 inhibitors.
- These drugs may have side effects such as myopathy, liver and kidney damage, and gastrointestinal discomfort and may interact with other medications such as anticoagulants and immunosuppressants.
Future therapies
- Several new treatments are being developed to target the cholesterol synthesis and regulation pathway, such as inhibitors of SREBP activation, RNA interference of PCSK9 expression, and gene therapy for genetic disorders.
- These therapies may provide new options for treating hypercholesterolemia and other related diseases.
Frequently Asked Questions (FAQs)
What is normal cholesterol?
Normal cholesterol is the level of cholesterol in the blood that is considered healthy and not associated with an increased risk of cardiovascular disease. The usual range of cholesterol is typically defined by the levels of low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and total cholesterol in the blood.
What is the role of cholesterol?
Cholesterol plays a critical role in maintaining cell membranes’ structural integrity and fluidity. Cholesterol also acts as a precursor molecule for the synthesis of several essential compounds in the body, including steroid hormones, bile acids, and vitamin D. In addition, cholesterol is involved in the transport of lipids and other molecules in the bloodstream.
What are the primary sources of cholesterol?
The body can produce its cholesterol in the liver, but it can also be obtained from dietary sources, such as animal-based foods like meat, dairy, and eggs. The consumption of high amounts of saturated and trans fats can lead to increased levels of cholesterol in the body.
What type of hormone is cholesterol?
Cholesterol is not a hormone, but it is a precursor molecule for synthesizing several essential hormones, including testosterone, estrogen, and cortisol. These hormones are classified as steroid hormones and are synthesized from cholesterol in various tissues in the body.
What are two types of cholesterol?
The two main types of cholesterol are low-density lipoprotein (LDL) and high-density lipoprotein (HDL). LDL cholesterol is often referred to as “bad” cholesterol because it can contribute to plaque buildup in the arteries. In contrast, HDL cholesterol is often referred to as “good” cholesterol because it can help remove excess cholesterol from the bloodstream.
What is the complete form of VLDL?
The complete form of VLDL is very low-density lipoprotein. VLDL is a type of lipoprotein produced in the liver and contains high levels of triglycerides. VLDL is involved in transposing triglycerides and other lipids into the bloodstream.
Conclusion
Cholesterol synthesis and regulation are complex and dynamic processes that involve multiple enzymes, genes, receptors, and signaling pathways.
Understanding cholesterol synthesis’s mechanisms and clinical implications are crucial for maintaining our health and developing new therapies for related disorders.
This article aims to help readers improve their knowledge and awareness of this important topic by providing comprehensive and accurate information on cholesterol synthesis.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.