The pancreas is a vital organ that plays an essential yet often overlooked role in maintaining health through the production of hormones. Though small, the pancreas is powerful when regulating glucose metabolism, food digestion, and other key bodily processes. This guide will provide a comprehensive overview of the pancreas and its secretion of critical hormones like insulin, glucagon, somatostatin, and pancreatic polypeptide (PP).
The pancreas was first identified for western civilization by Herophilus (335–280 BC), a Greek anatomist and surgeon. Only a few hundred years later, Rufus of Ephesus, another Greek anatomist, gave the pancreas its name. The pancreas secrets three different peptide hormones. They are Insulin, Glucagon and Stomatostatin.
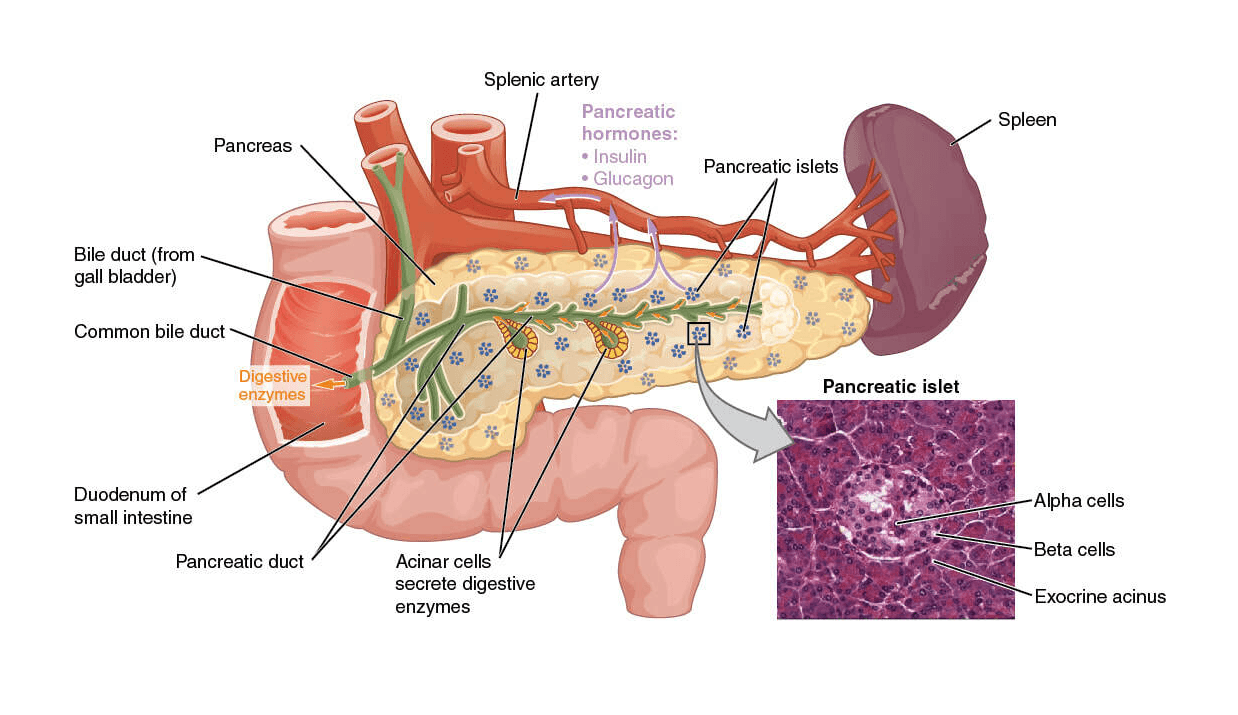
The pancreas is a glandular organ in the abdomen, positioned behind the stomach. It contains clusters of cells known as the islets of Langerhans responsible for the endocrine function of the pancreas – which involves the production and secretion of hormones into the bloodstream.
These pancreatic hormones are indispensable in regulating blood sugar, digestion, appetite, and metabolism. The four main hormones secreted by the pancreatic islets include:
- Insulin: Lowers blood glucose levels by promoting the uptake of glucose into cells
- Glucagon: Raises blood glucose levels by stimulating glucose release
- Somatostatin: Regulates pancreatic hormone production
- Pancreatic Polypeptide (PP): Aids in the regulation of pancreatic and gastrointestinal secretions
Imbalances in pancreatic hormone levels can lead to serious medical conditions like diabetes and pancreatic cancer. That’s why it’s important to understand how these hormones work together to maintain homeostasis and health.
This guide will provide a deep dive into pancreatic anatomy, the distinct functions of the key pancreatic hormones, their regulation, and associated disorders:
The Pancreas: Anatomy and Function
The pancreas is an oblong organ measuring around 15 to 20 cm long that sits deep in the abdomen, behind the stomach. Other organs surround it, including the spleen, small intestine, liver, and gallbladder.
- The pancreas (from pankreas: panG=all, kreasG=flesh); offering to the fleshy nature of the tissue) is both exocrine & endocrine gland.
- It locates the below the stomach between the curve of duodenum & spleen.
- It is a compact & lobulated organ.
- The pancreas composed of two types of cell.
- The pancreas secretes peptide hormones.
- Pancreatic hormones are peptide hormones
Structurally, the pancreas contains two key components:
- Exocrine tissue makes up over 95% of pancreas mass and secretes digestive enzymes into ducts, leading the small intestine to break down fats, proteins, and carbohydrates from food.
- Endocrine tissue makes up only 1-2% of pancreatic mass in the form of pancreatic islets (islets of Langerhans). It secretes hormones like insulin into the bloodstream to regulate glucose and metabolic processes.
This guide will focus on the endocrine function of the pancreas and its secretion of hormones like insulin and glucagon.
1. Glandular cells (or) Acinar (or) Acinii (exocrine):
The cells make up the bulk of the pancreatic tissues & secrete digestive juices into the duodenum by the pancreatic duct.
2. Polygonal cells (or) islets of langerhans (or) islet tissue (endocrine):
Its secretion releases into the blood directly. These were discovered by “Langerhans” in 1867. The islets of Langerhans in mammals contain three major types of cells, they are a-cells, b-cells, g-cells.
- alpha-cells –> Secretes – “Glucagon” hormones
- beta-cells –> Secretes – “Insulin” hormones
- gamma-cells –> Secretes-“Somatostatin” hormone
Endocrine vs. Exocrine Function of the Pancreas
The pancreas has a unique dual role in the human body. It acts as both an endocrine gland secreting hormones and an exocrine gland secreting digestive enzymes.
Endocrine function involves the release of hormones like insulin and glucagon into the bloodstream by clusters of endocrine cells, influencing processes like glucose metabolism.
Exocrine function involves the secretion of pancreatic juices containing digestive enzymes (like amylase, lipase, and trypsin) through ducts into the small intestine to break down food.
Though the endocrine and exocrine systems of the pancreas work independently, some interplay between digestion and hormone release aids in maintaining balance. However, the endocrine function will be emphasized in this guide for its role in regulating glucose and hormone levels.
a. Insulin – The Blood Sugar Lowering Hormone
Insulin is a critical peptide hormone secreted by beta cells in the pancreas. It is indispensable in lowering blood glucose levels and allowing cells throughout the body to use glucose for energy.
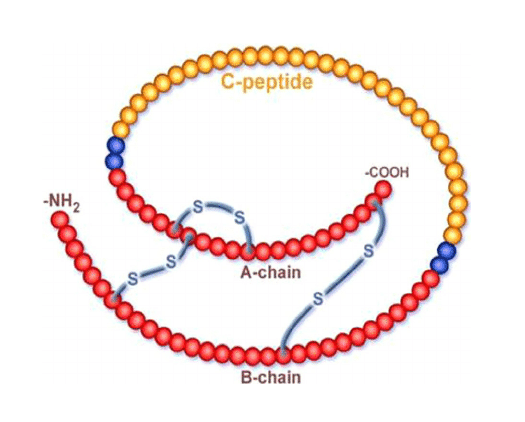
When blood glucose levels rise after eating a meal, the beta cells of the pancreas are triggered to release insulin into the bloodstream. Insulin then acts as a key that unlocks cell membranes, allowing glucose to enter cells. It stimulates cells, such as fat and muscle cells, to absorb excess glucose from the blood and store it as glycogen.
This way, insulin regulates blood sugar, preventing hyperglycemia (high blood glucose). It also stimulates the uptake of amino acids into cells, allowing proteins and fats to be synthesized.
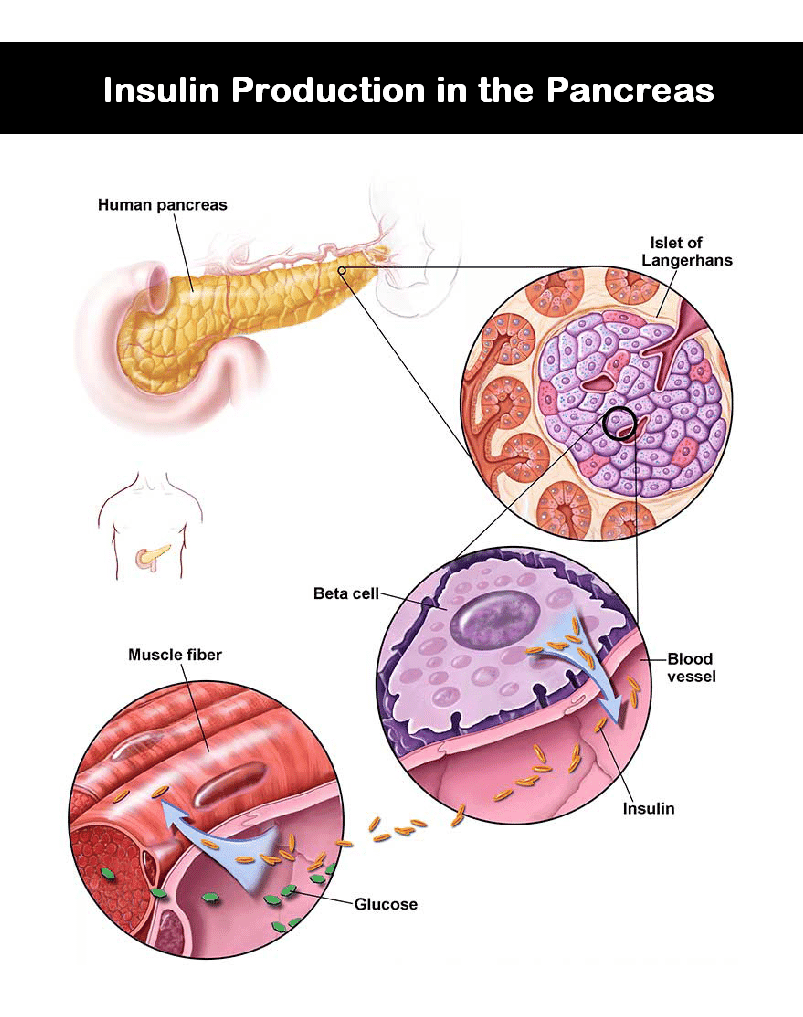
Insulin is chiefly responsible for maintaining glucose homeostasis and normal metabolism. Insufficient insulin production or sensitivity can lead to unchecked high blood sugar, a condition known as diabetes mellitus.
b. Glucagon: The Blood Sugar Raising Hormone
Glucagon is another vital pancreatic hormone secreted by alpha cells of the pancreas. It counterbalances the action of insulin, raising blood glucose levels when they fall too low.

When blood sugar drops, such as during prolonged exercise or fasting, alpha cells in the pancreas are triggered to release glucagon into circulation. It stimulates the breakdown of glycogen stored in the liver into glucose, releasing it back into the bloodstream.
Glucagon also stimulates lipolysis, the breakdown of fats into fatty acids, providing an alternative energy source. It prevents blood sugar from falling to dangerously low levels, known as hypoglycemia.
Therefore, through opposing actions, glucagon and insulin work together to maintain optimal blood glucose levels. This endocrine feedback loop is essential for glucose homeostasis.
c. Somatostatin: The Hormone-Inhibiting Hormone
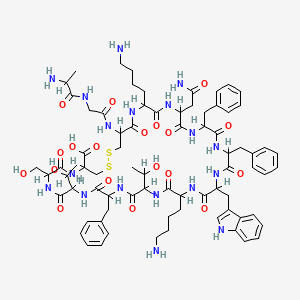
Somatostatin, also known as growth hormone-inhibiting hormone (GHIH), is a peptide produced and secreted by delta cells in the pancreas and other organs. It plays a key regulatory role, inhibiting the release of several gastrointestinal and pancreatic hormones, including:
- Insulin
- Glucagon
- Gastric acid
- Absorption of nutrients like glucose
- Secretin
By preventing the over secretion of hormones, somatostatin helps maintain metabolic equilibrium. It is also found in the nervous system and cerebrospinal fluid, inhibiting neurotransmission.
Synthetic forms of somatostatin called somatostatin analogs can help treat some hormone-secreting tumors like thyroid cancer, acromegaly, and neuroendocrine tumors. The inhibition of gastric acid secretion also makes it useful for treating ulcers.
d. Pancreatic Polypeptide (PP) – Appetite and Digestion Regulator
Pancreatic polypeptide (PP) is another peptide hormone secreted by PP cells in the endocrine pancreas, primarily in response to food consumption. Though its functions are not entirely clear, PP is thought to play a role in:
- Regulating pancreatic secretions
- Inhibiting gallbladder contractions
- Regulating gastrointestinal motility
- Stimulating appetite suppression
Research indicates that PP may influence digestion by slowing gastric emptying and intestinal motility. It also reduces appetite through hypothalamic signaling.
Abnormal PP levels have been associated with conditions like diabetes and pancreatic cancer. However, more studies are still needed to understand this little-known pancreatic hormone’s regulatory roles fully.
Regulation of Pancreatic Hormones
The secretion of pancreatic hormones like insulin and glucagon is tightly regulated through a delicate balance of stimulatory and inhibitory factors. Here is an overview of how some key players help maintain optimal hormone levels:
Blood Glucose Levels
- Rising blood glucose stimulates insulin secretion and inhibits glucagon release
- Falling blood glucose stimulates glucagon secretion and inhibits insulin release
Nervous System Input
- Stimulation of the parasympathetic nervous system promotes insulin secretion
- Stimulation of the sympathetic nervous system inhibits insulin secretion
- GLP-1 and leptin stimulate insulin release
- Ghrelin inhibits insulin secretion
Somatostatin
- Somatostatin inhibits both insulin and glucagon release
Fatty Acids
- Increased fatty acids promote insulin secretion
This multi-level regulation prevents prolonged over- or under-secretion of hormones like insulin and glucagon, maintaining blood glucose homeostasis.
Disorders and Conditions Related to Pancreatic Hormones
Since pancreatic hormones like insulin and glucagon play such a vital role in glucose regulation and metabolism, imbalances can lead to several hormonal and endocrine disorders:
a. Diabetes Mellitus
Diabetes is characterized by high blood glucose levels due to inadequate insulin production or sensitivity, resulting in poor glucose uptake by cells. The main types include:
- Type 1 diabetes: autoimmune destruction of insulin-producing beta cells leads to insulin deficiency
- Type 2 diabetes: cells become insulin resistant, failing to respond to normal insulin levels
Both types disrupt normal glucose homeostasis, leading to hyperglycemia and long-term complications if left uncontrolled. Diabetes management aims to normalize blood glucose levels through insulin therapy, medications, diet, and lifestyle changes.
b. Hormone Secreting Tumors
Pancreatic neuroendocrine tumors arising in islet cells can abnormally produce excess hormones like insulin, leading to complications:
- Insulinomas – Insulin-secreting tumors cause hypoglycemia
- Glucagonomas – Glucagon-secreting tumors raise glucose levels
- Treatment may involve surgical removal and somatostatin analogs.
c. Pancreatitis
Inflammation of the pancreas (pancreatitis) can impair the production and secretion of insulin and other hormones, potentially leading to diabetes. Causes include gallstones, alcohol abuse, and genetic factors. Treatment involves hospitalization, IV fluids, pain management, and medications.
Frequently Asked Questions About Pancreatic Hormones
Here are answers to some frequently asked questions about pancreatic hormones:
Which cells in the pancreas produce insulin?
Insulin is produced by beta cells located within clusters of endocrine cells in the pancreas called the islets of Langerhans.
How can I tell if I have insulin resistance?
Warning signs of insulin resistance include increased hunger, fatigue, excessive thirst, blurred vision, slow wound healing, and dark skin patches. A physician can confirm insulin resistance through blood tests.
Does alcohol affect insulin levels?
Heavy alcohol consumption can reduce insulin secretion and sensitivity, potentially contributing to diabetes. Moderate alcohol intake does not appear to impact insulin significantly.
What foods help increase insulin sensitivity?
Foods that may help improve insulin sensitivity include fatty fish, leafy greens, apple cider vinegar, berries, cinnamon, and foods high in magnesium like almonds, spinach, and beans.
Can stress affect insulin levels?
Yes, chronic stress promotes the release of hormones like cortisol and epinephrine that can raise blood glucose and alter insulin levels. Stress management through exercise, meditation, and therapy can help stabilize insulin.
Conclusion
In summary, the pancreas plays a central yet underappreciated role in maintaining metabolic health by secretion of key hormones like insulin, glucagon, somatostatin, and pancreatic polypeptide from clusters of specialized cells called the islets of Langerhans.
The proper functioning of these hormones is essential for regulating glucose levels, digestion, appetite, growth, and energy metabolism. Imbalances can lead to hormone disorders like diabetes and cancer. Further understanding and research into pancreatic hormones will provide insights into optimizing health and developing treatments.
This guide aimed to shed light on the critical functions of our amazing pancreas. Its ability to dynamically regulate hormones reveals the incredible coordination within our bodies despite the complexities of metabolism, digestion, and energy needs. Appreciating this should inspire further curiosity into the intricacies of physiology.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.




