The thyroid gland is a small, butterfly-shaped organ located at the base of the neck. It produces two main thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – that regulate metabolism, growth, development, and many other essential body functions.
Thyroid hormones play a crucial role in regulating vital body processes and maintaining overall health and wellbeing. An understanding of how the thyroid gland functions and the critical importance of thyroid hormones can help prevent disorders that affect millions of people worldwide.
What are Thyroid Hormones?
Thyroid hormones, as the name suggests, are a group of chemical messengers produced by the thyroid gland, a butterfly-shaped gland located in the neck, just below the Adam’s apple.
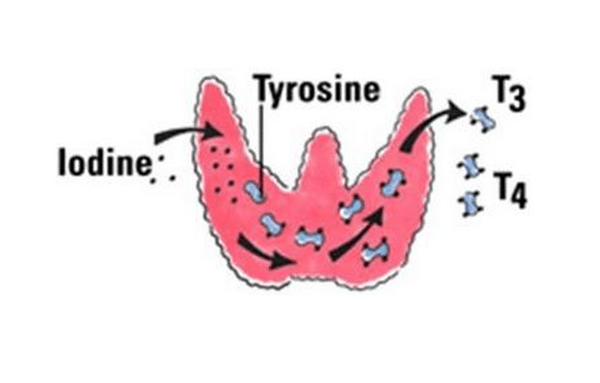
The thyroid gland is responsible for synthesizing two primary thyroid hormones: T3 (triiodothyronine) and T4 (thyroxine). These hormones are synthesized using iodine and are instrumental in orchestrating a wide array of bodily functions, essentially acting as the body’s metabolic regulators.
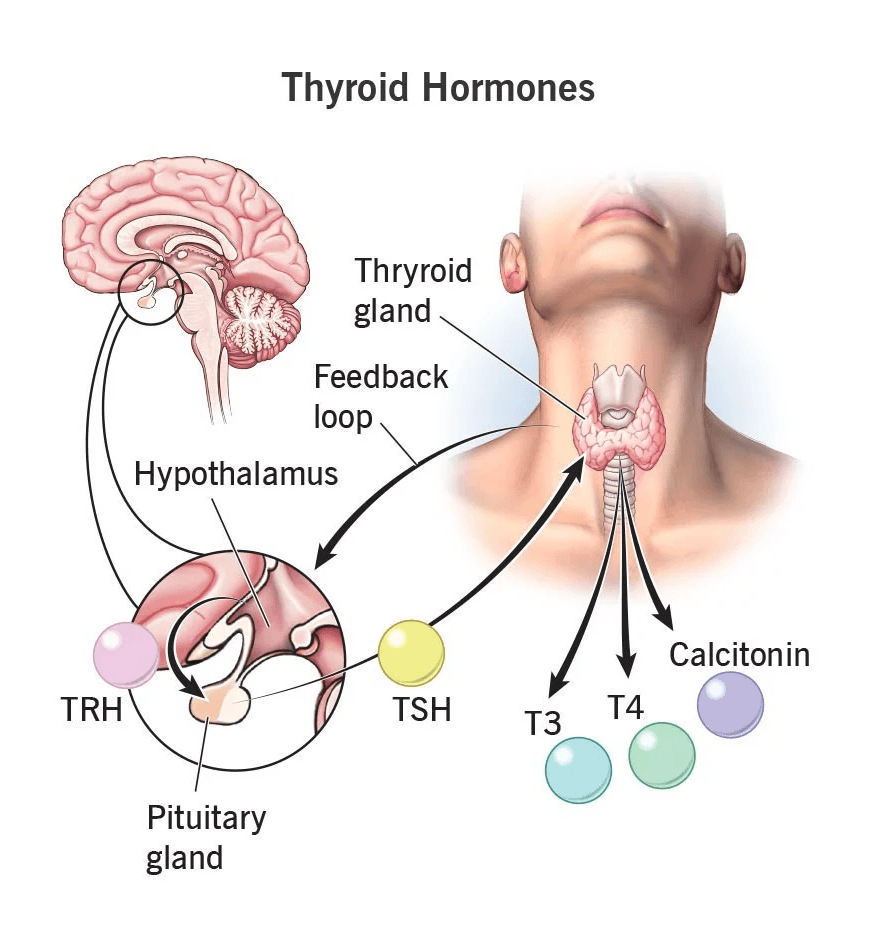
Hypothalamus releases thyrotropin-releasing hormone (TRH) that stimulates the secretion of TSH in the pituitary gland.
Iodine is the critical ‘ingredient’ for the production of thyroid hormones.
Thyroid hormones are a group of hormones produced by the thyroid gland, primarily composed and in the blood is usually distributed as follows:
- T3 (Triiodothyronine)
- T4 (Thyroxine): It is the main form of thyroid hormone circulating in the blood.
These hormones travel through the bloodstream to reach every cell in the body and control the speed of metabolic functions.
The Importance of Thyroid Hormones
The significance of thyroid hormones within the body cannot be overstated. These hormones are essentially the conductors of the body’s metabolic orchestra, ensuring that various processes operate harmoniously. Here are some of the key areas in which thyroid hormones play pivotal roles:
- Metabolism Regulation: Thyroid hormones have a direct impact on the body’s metabolism, influencing the rate at which cells convert nutrients into energy. This regulation is essential for maintaining a healthy weight and ensuring that energy production and expenditure are in balance.
- Role in Growth and Development: In children and adolescents, thyroid hormones are crucial for proper growth and development, including the development of the brain, bones, and other tissues. They continue to support tissue maintenance and repair in adults.
- Impact on Body Temperature:Thyroid hormones help control body temperature, ensuring that it stays within a narrow and healthy range. Imbalances in these hormones can lead to sensitivity to temperature changes and may result in symptoms like cold intolerance or excessive sweating.
Understanding the fundamental importance of thyroid hormones in maintaining overall health provides the basis for delving into the intricate workings of these hormones, their role in various bodily functions, and the potential consequences of imbalances or disorders related to the thyroid gland. In the sections that follow, we will explore the thyroid gland’s anatomy, the types of thyroid hormones produced, and their vital functions in greater detail.
Thyroid hormones are essential for:
- Regulating metabolism and energy production
- Controlling appetite and body weight
- Driving protein production
- Managing cholesterol levels
- Supporting heart health
- Regulating menstrual cycles
- Ensuring proper growth and development, especially in children
- Influencing muscle strength
- Maintaining bone health
- Regulating body temperature
- Impacting mood and mental health
- Influencing central nervous system function
When thyroid hormone levels are not optimal, all of these processes can be disrupted, leading to impaired wellbeing and increased disease risk.
The Thyroid Gland
Thyroid hormones play a crucial role in regulating various aspects of our health. The thyroid gland, a butterfly-shaped endocrine gland located at the base of the neck, is responsible for producing these hormones. Its normal function is to release thyroid hormones into the bloodstream, where they act as messengers to control the amount of thyroid hormones in the body.
a. Thyroid Gland Location
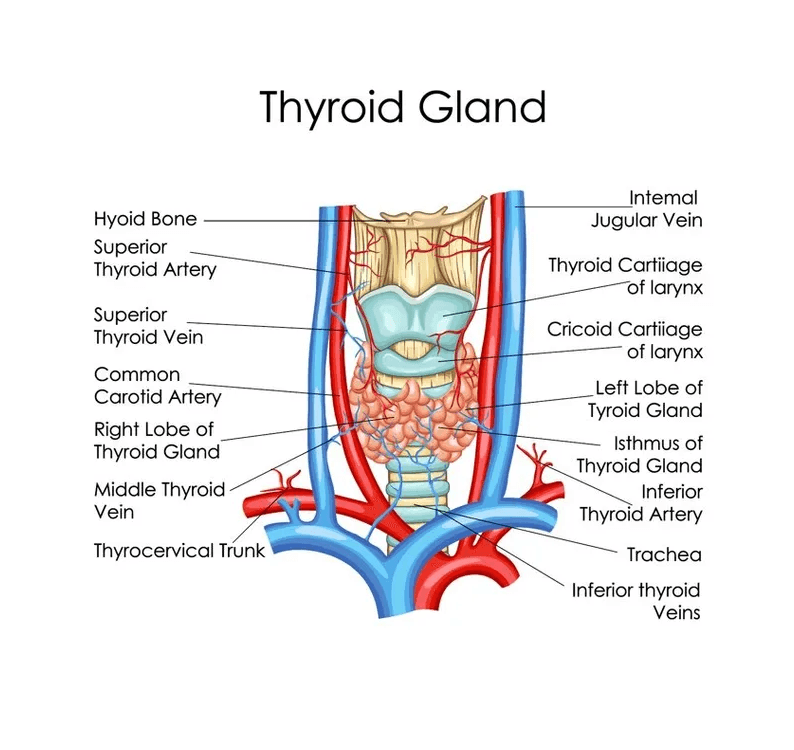
The thyroid gland is located at the base of the front of the neck, just below the larynx (voice box) and above the trachea (windpipe). It wraps around the trachea with a narrow band of tissue called the thyroid isthmus connecting its two lobes.
The thyroid’s position in the neck allows it to access the bloodstream to release hormones and receive feedback from the hypothalamus and pituitary gland. Its location lets physicians palpate the gland to check for enlargement or nodules.
The thyroid gland secretes hormones that have far-reaching effects on the body’s metabolism and well-being.
b. Thyroid Gland Size and Shape
The thyroid gland has a butterfly-like shape formed by two lobes connected by the thyroid isthmus. It is about 5 cm long, 3 cm wide, and 2 cm thick.
Each lobe is a pinkish-red, highly vascular structure composed of specialized follicular cells that produce and store thyroid hormones. The isthmus spans the trachea to join the two lobes together.
The thyroid enlarges during puberty and pregnancy to increase hormone production. It may also enlarge in hyperthyroid conditions or due to nodules and tumors.
c. Thyroid Gland Anatomy
The thyroid gland is a small, butterfly-shaped organ located at the base of the front of the neck.
Here are the key anatomical features of the thyroid gland:
- The thyroid gland has two lobes, a right lobe and a left lobe, that are connected together by a narrow band of tissue called the isthmus. This gives the thyroid gland a butterfly-like appearance.
- Each lobe is about 5 cm long, 3 cm wide, and 2 cm thick. The two lobes lie on either side of the trachea (windpipe).
- The isthmus spans across the trachea to connect the two lobes together. It is about 1-2 cm wide.
- The thyroid gland wraps around the sides of the trachea. It extends from the lump in the throat called the laryngeal prominence down to the second or third tracheal ring.
- The thyroid gland is located below the thyroid cartilage (Adam’s apple) and above the sternum and clavicles.
- It is enveloped by a thin fibrous capsule. Inside, it is composed of many small spherical sacs called thyroid follicles.
- The thyroid follicles consist of a central colloid surrounded by follicular cells. The colloid stores the precursor thyroid hormone thyroglobulin.
- Four parathyroid glands, which control calcium levels, are also located on the posterior surface of the thyroid lobe.
- Several muscles are attached to the thyroid, including the sternohyoid, sternothyroid, and omohyoid muscles. These help anchor the gland in place.
- The thyroid gland has an extensive blood supply from the superior and inferior thyroid arteries. It also has a rich lymphatic drainage.
- Nerve supply to the thyroid gland comes from the superior, middle, and inferior cervical ganglion of the sympathetic trunk.
The thyroid gland has a butterfly shape with two lobes, multiple follicles that produce hormones, and is located at the front of the neck below the larynx and above the trachea. Its position and blood supply allow optimal production and release of thyroid hormones.
d. Thyroid Gland Blood Supply
The thyroid gland has an extensive blood supply from two arteries:
- Superior thyroid artery: Branch of the external carotid artery
- Inferior thyroid artery: Branch of the subclavian artery
This ample blood flow allows efficient delivery of raw materials like iodine and tyrosine needed for synthesizing T3 and T4 hormones.
e. Thyroid Gland Histology
The basic functional unit of the thyroid gland is the thyroid follicle. Follicles are composed of:
- Follicular cells: the thyroid hormones T3 and T4
- Parafollicular cells (C-cells): Produce calcitonin hormone
- Colloid: Inner follicle material rich in thyroglobulin protein
Thyroid hormones are synthesized and stored as a complex with thyroglobulin pending release into the bloodstream.
f. Thyroid Supporting Structures
The thyroid gland is supported and held in place by essential structures:
- Thyroid cartilage: Provides anterior protection
- Trachea and larynx: Anchor the gland in place
- pre-tracheal fascia: Connective tissue supporting the gland
- Strap muscles: Muscles helping hold the gland (sternohyoid, sternothyroid)
g. Thyroid Embryonic Development
The thyroid gland begins forming during the 3rd-4th weeks of embryonic development from two structures:
- Thyroglossal duct: Gives rise to the thyroid isthmus
- Ultimobranchial body: Forms the lateral thyroid lobes
Congenital thyroid defects can sometimes occur when this complex development goes awry.
From its strategic position in the neck to its unique cellular composition, the structure of the thyroid gland provides an intriguing insight into how it manufactures and secretes thyroid hormones.
Understanding the anatomy and embryology of the thyroid facilitates a better appreciation of thyroid disorders and treatments. The intricacy of the thyroid reflects the importance of the hormones it produces in regulating some of the body’s most vital functions.
Types of Thyroid Hormones
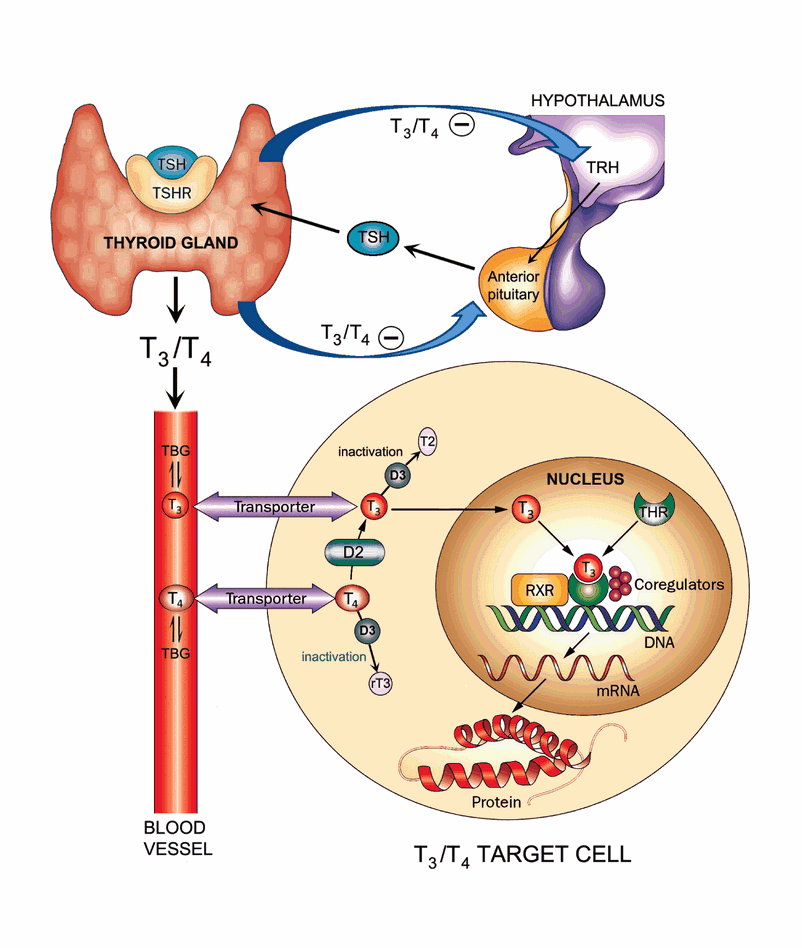
The pituitary gland in the brain is a key player in this intricate system. It releases thyroid-stimulating hormone (TSH) to tell the thyroid gland to produce more or less thyroid hormone as needed. An overactive thyroid gland is often linked to elevated TSH levels.
The two primary thyroid hormones are T3 (triiodothyronine) and T4 (thyroxine).
a. T3 or Triiodothyronine
- T3 contains three iodine atoms and is the more biologically active thyroid hormone.
- It influences cellular metabolism and energy production.
- T3 is produced both directly by the thyroid gland and from conversion of T4 in tissues.
- Only about 20% of T3 comes directly from the thyroid gland.
b. T4 or Thyroxine
- T4 contains four iodine atoms and is less biologically active than T3.
- It must be converted to T3 to exert effects on cells.
- About 80% of the thyroid gland’s hormone production is T4.
Both T3 and T4 work together to regulate essential bodily processes and must remain in balance.
What are Normal Thyroid Hormone Levels?
Normal thyroid hormone levels can vary slightly depending on the laboratory and the specific tests being conducted. However, in general, the typical reference ranges for thyroid hormone levels are as follows:
- TSH (Thyroid-Stimulating Hormone): The normal range for TSH levels is typically between 0.4 to 4.0 mU/L (milli-international units per liter). TSH is produced by the pituitary gland and stimulates the thyroid gland to produce thyroid hormones.
- Free T4 (Free Thyroxine): Free T4 levels usually fall within the range of 0.9 to 1.8 ng/dL (nanograms per deciliter). Free T4 is the active form of thyroxine, one of the main thyroid hormones.
- Free T3 (Free Triiodothyronine): The normal range for free T3 levels is typically between 2.3 to 4.2 pg/mL (picograms per milliliter). Free T3 is the active form of triiodothyronine, another important thyroid hormone.
It’s important to note that these reference ranges can vary slightly from one lab to another, so it’s essential to interpret your results in the context of the specific reference range provided by the laboratory that conducted the tests.
Additionally, “normal” thyroid hormone levels can vary from person to person, and what’s considered normal for one individual may not be the same for another. It’s important to consult with a healthcare provider who can interpret your test results in the context of your overall health and medical history.
If you have concerns about your thyroid hormone levels, it’s best to discuss them with a healthcare professional who can provide personalized guidance and treatment if necessary.
Synthesis & secretion of thyroxin (or) thyroid gland secretion:
Thyroid hormone metabolism is a complex process that involves the production and utilization of these hormones. The hormones secreted by the thyroid gland play a critical role in numerous bodily functions. They act as messengers, helping to regulate how hormones in the body become free hormone or bound to carrier proteins.
Step 1: Uptake of iodine
- Thyroid gland takes up and concentrates iodine. It can concentrate iodine up to 10,000 times.
- The was originally thought to be linked to Na+/K+-ATPase, but now another Na+/I– symporter carrier system is also proposed.
- This step is inhibited by thiocyanate and perchlorate, which compete for the carrier mechanism. This step is stimulated by TSH (thyroid stimulating hormone).
- There is a congenital defect associated with this step. It is called iodine-trapping defect and may be treated by large doses of iodine.
Step 2: Oxidation of Iodine
- The iodine taken up by the thyroid cell is oxidized to active iodine.
- The thyroid cell is oxidized to active iodine. The thyroid is the only organ, which can perform this oxidation step. This is catalyzed by the enzyme “Thyroperoxidase, tetrameric protein with molecular weight 60,000.
- The reaction needs hydrogen peroxide, which is produced by an NADPH-dependent reaction. The NADPH is generated by the hexose monophosphate shunt pathway.
- This second step is stimulated by TSH (thyroid-stimulating hormone) and inhibited by antithyroid drugs such as thiourea, thiouracil some patients with an inborn error of iodine oxidation defect, which may be treated by T4 administration.
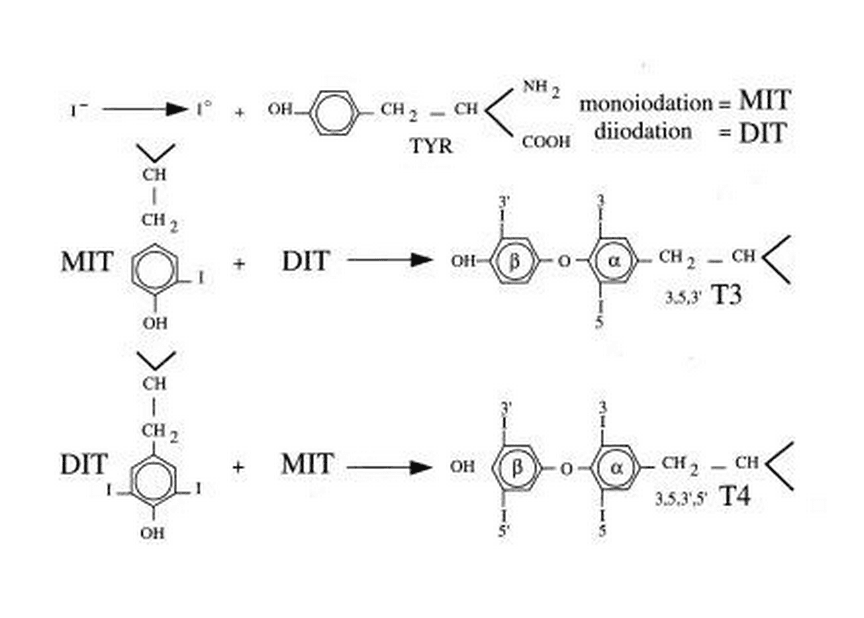
Step 3: Iodination
- Then thyroglobulin (Tgb) is iodinated. Thyroglobulin is synthesized by the thyroid follicular cells.
- It is a large protein with about 5000 amino acids (660kD).
- It contains about 10% carbohydrates. There are 115 tyrosine residues in the Tgb, out of which 35 residues can be iodinated.
- Iodination of the tyrosine is taking place on the intact Tgb molecule in the follicular space. Thus, mono-iodotyrosine (MIT) and di-iodotyrosine (DIT) are produced.
Step 4: Coupling
- Some of the tyrosine residues in the thyroglobulin are aligned opposite each other, and are coupled.
- When two DIT molecules couple, one molecule of tetra-iodothyronine (T4) is formed.
- The triiodothyronine (T3) may be formed either by coupling of one MIT with one DIT (or) more commonly, by deiodination of T4.
- Under normal conditions, 99% of the hormone produced by the thyroglobulin molecule. The iodination and coupling are taking place in the borders of the follicular cells.
- The iodotyrosine coupling defect, an inborn error, affects this 4th step. Treatment is to give T4.
Step 5: Storage
- The thyroid gland is unique, in that it is the only endocrine gland to store appreciable amounts of the hormone (step4 in figure).
- The stored Tg contains about eight T4 residues per molecule.
Step 6: Utilization
When necessity arises, the thyroglobulin is taken from the acinar colloid, back into the cell by pinacocytosis.
Step 7: Hydrolysis
- The T4 is liberated by hydrolysis by specific proteases.
- TSH markedly enhances this activity. This hydrolysis is depressed by iodine and therefore potassium iodide (KI) is used as an adjuvant in hyperthyroidism.
- In a genetic disorder, abnormal Tgb is synthesized, resulting in deficient proteolysis and deficiency of thyroxine.
Step 8: Release
- The T4 thus generated is released into the bloodstream. The T3 is produced by de-iodination at 5’ position, either inside the thyroid cell (or) in the peripheral tissues.
- The reverse T3 (rT3) is produced by de-iodination at 5’ position. Its biological activity is negligible.
Step 9: Salvage of iodine
- The MIT and DIT that are not utilized are de-iodinated and salvaged for re-utilization inside the cell itself (step9 in figure).
- The inborn error of metabolism affecting this step is called the “deiodinase” defect. In such cases, DIT and MIT are seen in urine. Since iodine is excreted, iodine deficiency is manifested. Treatment is to give iodine.
Functions of Thyroid Hormones
The thyroid gland’s proper functioning and the regulation of thyroid hormones are crucial for maintaining health. Understanding the causes and effects of an overactive or underactive thyroid gland is vital, as it can have a significant impact on the body’s overall well-being.
Thyroid hormones influence virtually every cell and system in the body. Some of their most important roles include:
a. Metabolism Regulation
Thyroid hormones accelerate the basal metabolic rate. They:
- Increase carbohydrate absorption
- Boost protein synthesis
- Raise fat breakdown
This increases energy production and the rate at which calories are burned.
b. Growth and Development
Thyroid hormones are crucial for growth and maturation, especially in infants and children. They promote:
- Normal bone growth
- Nervous system development
- Pubertal changes
Congenital hypothyroidism can lead to cretinism and mental retardation.
c. Body Temperature Regulation
Thyroid hormones control thermoregulation by:
- Increasing heat production in tissues
- Raising basal body temperature
d. Cardiovascular Effects
T3 and T4 influence the heart and circulatory system by:
- Strengthening heart muscle contraction
- Lowering cholesterol levels
- Improving blood flow
e. Other Effects
Other key roles of thyroid hormones include:
- Regulating menstrual cycle and fertility
- Supporting central nervous system function
- Influencing mood, emotions, and mental health
- Impacting muscle strength and maintenance
- Maintaining bone density
- Affecting skin, hair, and nails
Thyroid Hormone Disorders
Abnormal levels of thyroid hormones lead to hypothyroidism and hyperthyroidism disorders.
a. Hypothyroidism
Hypothyroidism results from an underactive thyroid gland producing too little T3 and T4. Conversely, too little thyroid hormone, termed hypothyroidism, can result from a thyroid gland that isn’t functioning optimally. The thyroid gland may become underactive, and the levels of thyroid hormones in the blood can drop. In such cases, the pituitary gland in the brain releases thyroid-stimulating hormone (TSH) to tell the thyroid to produce more hormones.
Signs and Symptoms
Symptoms may include:
- Fatigue
- Weight gain
- Joint pain
- Constipation
- Dry skin and hair
- Intolerance to cold
- Depression
- Impaired memory
Causes
Causes include:
- Hashimoto’s thyroiditis
- Iodine deficiency
- Thyroid surgery
- Radiation treatment
- Congenital hypothyroidism
- Pituitary disorders
Treatment
Treatment involves thyroid hormone replacement drugs like levothyroxine.
b. Hyperthyroidism
Hyperthyroidism stems from an overactive thyroid producing excessive hormones.
When there is an abnormal thyroid function, problems can arise. Thyroid inflammation, or inflammation of the thyroid gland, can impact its ability to produce the right amount of thyroid hormones. Too much thyroid hormone, a condition known as hyperthyroidism, can stimulate the thyroid excessively, causing various health issues.
Signs and Symptoms
Symptoms may include:
- Weight loss
- Rapid heart rate
- Hand tremors
- Nervousness
- Heat intolerance
- Muscle weakness
- Irregular periods
Causes
Causes include:
- Graves’ disease
- Thyroid nodules
- Thyroiditis
- Excess iodine intake
Treatment
Treatments include antithyroid medications, radioactive iodine, and surgery.
c. Thyroid Autoimmune Diseases
Many thyroid conditions involve autoimmunity, including:
- Hashimoto’s thyroiditis
- Graves’ disease
- Postpartum thyroiditis
With autoimmunity, the immune system attacks and damages the thyroid gland. This leads to abnormal hormone levels.
Diagnosis of Thyroid Disorders
Thyroid function testing is a way to initially test thyroid function. It is done to measure the actual level of thyroid hormones in the body. Abnormal results usually indicate that the thyroid is producing too much or too little thyroid hormone.
It accurately reflects how the thyroid gland is controlled and helps diagnose conditions like medullary thyroid cancer, thyroid eye disease, or an overactive thyroid. Thyroid disorders are diagnosed through physical examination, blood tests, and imaging.
a. Symptoms and Signs
The physician will check for symptoms and signs pointing to hypo or hyperthyroidism. Palpation of the gland for enlargement or nodules is done.
b. Blood Tests
Blood tests help evaluate:
- TSH levels – elevated in hypothyroidism, low in hyperthyroidism
- Free T4 and T3 levels
- Thyroid antibodies in autoimmune conditions
c. Imaging Tests
Imaging like ultrasound or radioiodine scans can check thyroid structure and function.
d. Biopsy
A fine needle aspiration biopsy may be done on nodules to test for cancer.
Treatment of Thyroid Disorders
Treatment depends on the specific thyroid disorder and its severity.
a. Medications
- Levothyroxine replaces T4 in hypothyroidism
- Antithyroid drugs block thyroid hormone production in hyperthyroidism
- Radioactive iodine destroys overactive thyroid tissue
b. Lifestyle Changes
Dietary modifications, stress reduction, exercise, and other lifestyle factors can aid thyroid disorder treatment.
c. Surgery
For individuals with thyroid issues, thyroid hormone replacement therapy is often prescribed. This therapy helps maintain a healthy balance of thyroid hormones in the body. Understanding how thyroid hormones act, their role within the thyroid gland, and their metabolism is critical to managing thyroid conditions effectively. Surgery may involve complete or partial thyroidectomy. It is used for large goiters, nodules, or thyroid cancer.
d. Regular Monitoring
Lifelong thyroid function monitoring is crucial for best outcomes.
Importance of Thyroid Hormone Monitoring
Imbalances in thyroid hormones can have various causes. An overactive thyroid gland, for example, can lead to the thyroid producing too much thyroid hormone. Conversely, an underactive thyroid gland may not produce enough thyroid hormone. These conditions can result in an enlargement of the thyroid gland, which may be visible in a picture of the thyroid gland.
As thyroid disorders are chronic, ongoing monitoring of TSH, T3, T4 levels and thyroid examination are essential.
Who Needs Screening?
Routine TSH screening every 5 years is recommended starting at:
- Age 35 years
- Pregnancy
- High risk groups
More frequent monitoring is required for those on thyroid medications or with a history of thyroid disease.
Why Regular Monitoring Matters
Monitoring helps:
- Detect under or overtreatment
- Adjust medication dosages
- Check for recurrence of thyroid dysfunction
- Manage changes with age or health conditions
- Identify thyroid nodules or cancer early
Proper thyroid hormone balance is vital for wellbeing. The thyroid gland’s normal and abnormal functioning can significantly impact the release of thyroid hormones, affecting overall health. Regular thyroid function testing is a crucial way to monitor and maintain the health of this vital gland and the hormones it produces.”
Who is affected by thyroid disease?
Thyroid disease can affect people of all ages, genders, and backgrounds. It is a common medical condition, and the prevalence varies by the type of thyroid disorder. Here’s a breakdown of who can be affected by different thyroid conditions:
- Hypothyroidism: This condition, where the thyroid gland doesn’t produce enough thyroid hormones, can affect people of all ages, but it is more common in women, particularly those over the age of 60. It can also occur in infants and children (congenital hypothyroidism) and may result from autoimmune conditions like Hashimoto’s thyroiditis.
- Hyperthyroidism: An overactive thyroid gland, which produces an excess of thyroid hormones, can affect individuals of all ages and genders. Graves’ disease is the most common cause of hyperthyroidism, and it often affects women in their 20s and 30s.
- Thyroid Nodules: Thyroid nodules, which are growths on the thyroid gland, can occur in people of any age. They are more common as people get older, and women are more frequently affected.
- Thyroid Cancer: Thyroid cancer can affect individuals of any age, but it is most common in people between the ages of 25 and 65. Women are more likely to develop thyroid cancer than men.
- Autoimmune Thyroid Disorders: Conditions like Hashimoto’s thyroiditis and Graves’ disease, which are caused by autoimmune responses, can affect people of various ages and genders. They are more common in women, and they often develop during early to middle adulthood.
- Thyroid Disease in Pregnancy: Thyroid disorders can also affect pregnant women. It’s important to monitor thyroid function during pregnancy, as untreated thyroid disorders can have implications for both the mother and the developing baby.
It’s essential to recognize that thyroid diseases are widespread, and they can manifest at any stage of life. If you suspect you have a thyroid condition or have risk factors such as a family history of thyroid disease, it’s important to consult with a healthcare provider for proper evaluation, diagnosis, and treatment if necessary. Early detection and management can help individuals lead healthier lives despite thyroid disorders.
FAQs about Thyroid Hormones
What do thyroid hormones regulate in the body?
Thyroid hormones regulate metabolism, growth, development, body temperature, heart rate, cholesterol levels, mood, and other essential bodily functions. They influence almost every cell and organ system in the body.
What causes thyroid gland enlargement or goitre?
The most common causes of an enlarged thyroid gland or goitre include iodine deficiency, Hashimoto’s thyroiditis (autoimmune disorder), Grave’s disease (hyperthyroidism), thyroid nodules, and thyroid cancer. Pregnancy can also sometimes cause temporary thyroid enlargement.
What are the symptoms of hypothyroidism versus hyperthyroidism?
Hypothyroidism symptoms include fatigue, weight gain, feeling cold, constipation, muscle cramps, dry skin, hair loss, and depression. Hyperthyroidism causes weight loss, rapid heart rate, profuse sweating, hand tremors, irritability, muscle weakness, and difficulty sleeping.
How is hypothyroidism treated?
The standard treatment for hypothyroidism is daily oral administration of synthetic thyroid hormone medication such as levothyroxine. The dose is adjusted based on regularly monitoring TSH levels to maintain them within the normal range.
Are thyroid supplements helpful for thyroid health?
No evidence exists that supplements support thyroid function or help treat thyroid disorders in people with a normally functioning thyroid gland. However, ensuring adequate intake of iodine and selenium through food sources can help optimize thyroid hormone synthesis for those with certain deficiencies.
Conclusion
Understanding the thyroid gland and its crucial role in maintaining a normal thyroid function is essential for overall health. The thyroid gland releases thyroid hormones, and their levels in the blood are carefully regulated to ensure the body functions optimally.
Thyroid hormones T3 and T4 play an indispensable role in regulating metabolism, growth, temperature, cardiac function, emotions, fertility, and many other bodily processes. Diseases like hypothyroidism and hyperthyroidism can disrupt these critical functions and impair health and quality of life. Understanding thyroid gland anatomy, hormone physiology, disorders, and the importance of regular screening provides the knowledge needed for optimal thyroid health. With proper monitoring and treatment, thyroid conditions can be effectively managed.
Key Takeaways
- The thyroid gland produces T3 and T4 thyroid hormones that control vital body functions
- Hypothyroidism and hyperthyroidism are common thyroid disorders
- Symptoms, blood tests, and imaging diagnose thyroid disease
- Lifelong monitoring ensures ideal thyroid hormone levels
- With treatment, most people with thyroid disease can live normal, active lives
Thyroid hormones work behind the scenes to support robust health and wellness. Ensuring optimal thyroid function is a key part of maintaining overall wellbeing.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.
