Glucagon is a hormone that plays a crucial role in blood sugar regulation. It works with insulin to maintain normal blood glucose levels and ensure the body’s overall metabolic homeostasis. However, glucagon is often overlooked compared to the more well-known insulin. This article will provide a comprehensive overview of glucagon, including how it functions when released, its role in diabetes, potential weight loss benefits, and tips for maintaining healthy glucagon levels.
What is Glucagon?
Glucagon is a peptide hormone secreted by the alpha cells located in the pancreas. It belongs to a group of hormones known as pancreatic endocrine hormones, which include insulin and somatostatin.
Glucagon’s primary function is to raise blood glucose levels. It does this by stimulating the liver to break down glycogen into glucose and release it into the bloodstream. This process is called glycogenolysis.
Glucagon also promotes gluconeogenesis, glucose production from non-carbohydrate sources such as amino acids. Through these mechanisms, glucagon helps maintain normal blood sugar levels, especially during periods of fasting and starvation.

Chemistry of Glucagon Hormone
- Behrens and others first isolated glucagon in crystalline form. It is a peptide hormone with a molecular weight of 3,485.
- Glucagon hormone is made up of 29 amino acids arranged in a chain. Histidine is the first amino acid, and threonine is the last.
- Glucagon does not contain the amino acids cystine, proline, or isoleucine like insulin does. But it does have other amino acids like glutamine, asparagine, and arginine.
- Parenteral means giving something outside of the gastrointestinal tract. It includes injections under the skin, into the muscle, vein, or abdomen. Parenteral feeding is usually done intravenously.
Glucagon contains a small amount of sulfur from the amino acid methionine, not cystine.
The key points are:
- Glucagon hormone was first isolated by Behrens and others
- It is a peptide hormone weighing 3,485 daltons
- Made up of 29 amino acids in a chain
- Does not contain some amino acids found in insulin
- Parenteral means giving injections outside the GI tract
- Glucagon contains sulfur from methionine
Mechanism of Action
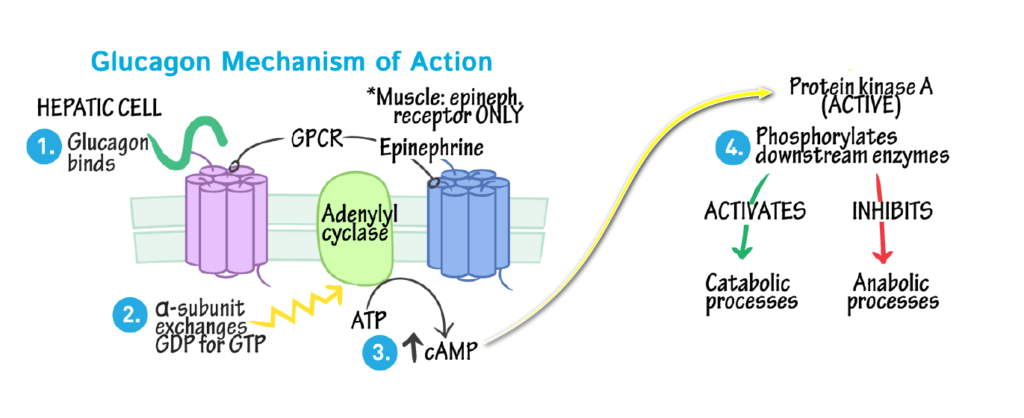
- The peptide hormone Glucagon combines with a membrane-bound receptor.
- The peptide hormone Glucagon activates the GDP-bound G-protein by converting it into GTP.
- The alpha subunit of G-protein now dissociates from the b and g subunits, and the unit binds to GTP.
- The GTP-G protein, in turn, activates adenyl cyclase. Thus, ATP is converted to cAMP.
- It combines with the regulatory subunit of the protein kinase.
- So, the catalytic sub-unit is free to act.
- The active protein kinase will phosphorylate the enzyme to activate glycogen phosphorylase.
In contrast, insulin has the opposite effect: it lowers blood glucose by facilitating sugar uptake from the blood into cells. Therefore, glucagon hormone and insulin work together to keep blood glucose within a normal range. Too much glucagon can lead to high blood sugar, while excessive insulin can cause dangerously low blood sugar.
Glucagon’s Role in Blood Sugar Regulation
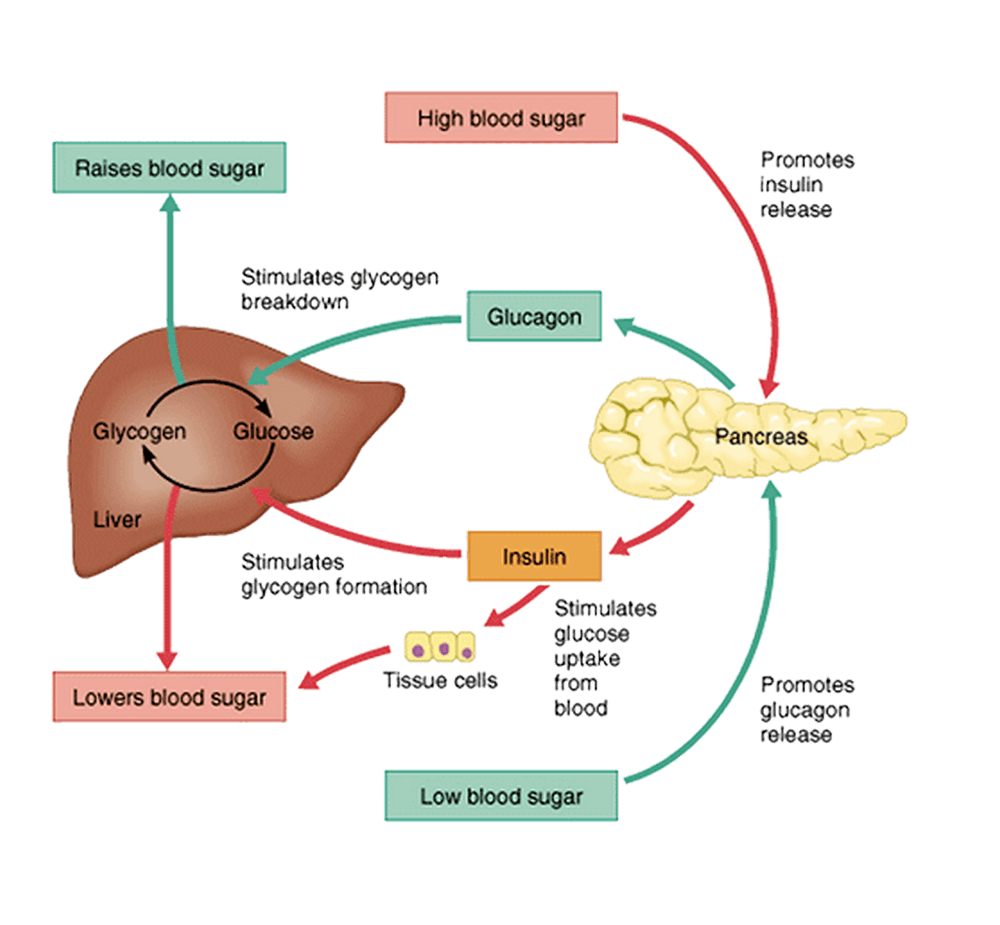
The main action of glucagon occurs in the liver. When blood glucose starts dropping, the alpha cells in the pancreas detect this and release glucagon.
Glucagon travels through the bloodstream and binds to glucagon receptors in liver cells. It triggers a series of events inside the cells:
- cAMP production is stimulated
- Protein kinase A is activated
- Phosphorylase kinase is activated
- Converts glycogen phosphorylase to its active form
Active glycogen phosphorylase then rapidly converts the stored glycogen into glucose-1-phosphate. Finally, glucose-1-phosphate is converted to free glucose and released from the liver cells into the circulation.
This cascading effect allows glucagon to mobilize glucose stores and elevate blood sugar levels quickly. Once released, glucagon hormone typically takes 5–15 minutes to act.
By stimulating glucose release, glucagon’s effect counters that of insulin. After a meal, insulin promotes glucose uptake and glycogen synthesis. Between meals, glucagon activates glycogen breakdown. This yin-yang relationship between the two hormones maintains blood glucose homeostasis.
When is Glucagon Released?
The main trigger for glucagon secretion is low blood glucose concentration. It typically occurs several hours after eating when blood sugar starts dropping. It also happens during fasting, starvation, and intense exercise.
When blood sugar dips below normal levels, glucagon release is stimulated to regain glucose. It prevents hypoglycemia.
Some of the primary stimuli that prompt alpha cells to discharge glucagon include:
- Hypoglycemia – low blood glucose
- Amino acids, especially alanine and arginine
- Intense aerobic activity
- Stress and adrenaline
- Low insulin levels
- Incretins: GIP and GLP-1
- Cholinergic activation: signals from the parasympathetic nervous system
Glucagon secretion is inhibited when blood glucose levels are elevated. Insulin and somatostatin from neighboring delta cells also suppress glucagon release after meals.
This feedback regulation allows glucagon to be released in a pulsatile manner; its levels fluctuate throughout the day depending on metabolic conditions. This pulsatile pattern is crucial for maintaining normal glucose homeostasis.
Glucagon in the Fasting State
Glucagon plays a vital role in glucose regulation during fasting and starvation.
When food isn’t ingested for several hours, blood glucose drops as insulin levels decrease and liver glycogen stores deplete. This reduction in blood sugar triggers glucagon secretion.
Glucagon then stimulates glycogenolysis and gluconeogenesis to provide glucose to vital tissues like the brain and heart. It releases glucose from the liver to serve as the main energy source for the body.
Without glucagon, fasting blood glucose could fall dangerously low. So, glucagon prevents hypoglycemia between meals and during extended periods of fasting. It fuels the brain and enables the body to function normally, even without food intake.
However, long-term fasting eventually leads to very low insulin and high glucagon levels. It can cause excessive glycogen breakdown, gluconeogenesis, and ketone production. Ketosis and ketoacidosis may develop if fasting is prolonged.
Glucagon Hormone and Diabetes
Glucagon plays a significant role in the pathophysiology and treatment of diabetes mellitus. Both type 1 and type 2 diabetes involve dysregulation of glucagon secretion and action.
In type 1 diabetes, the pancreas cannot produce insulin due to the autoimmune destruction of beta cells. It leads to insulin deficiency and hyperglycemia. Glucagon levels are also abnormally elevated in type 1 diabetes. It further contributes to high blood glucose.
Type 2 diabetes also demonstrates impaired glucagon secretion. In the beginning stages, glucagon levels are often inappropriately increased after meals. It promotes excessive hepatic glucose output and aggravates hyperglycemia.
As type 2 diabetes advances, alpha cell responsiveness diminishes. Glucagon levels fail to increase sufficiently in response to hypoglycemia. It can cause more frequent and severe hypoglycemic episodes.
Several diabetes treatments target glucagon activity:
- GLP-1 agonists: These medications stimulate insulin release but also suppress glucagon secretion.
- SGLT2 inhibitors: These oral agents reduce blood glucose while simultaneously lowering glucagon levels.
- Pramlintide: This synthetic version of amylin delays gastric emptying and inhibits postprandial glucagon release.
- Glucagon antagonists: Experimental drugs that block glucagon receptors are being developed.
- Artificial pancreas: closed-loop insulin pump systems can automate insulin and glucagon delivery.
Better understanding and control of dysregulated glucagon represents an important focus for improving diabetes care.
Glucagon and Weight Loss
Due to its effects on appetite and metabolism, glucagon is being explored as a potential weight-loss treatment.
Glucagon suppresses appetite by slowing gastric motility and increasing satiety. It is likely mediated through the central nervous system. Glucagon also increases resting energy expenditure and fat oxidation.
Some researchers hypothesize that glucagon administration may promote weight loss through these mechanisms. Early studies in rats and humans demonstrated that glucagon injections over 1-4 weeks could reduce food intake and cause significant weight loss.
However, the weight loss was temporary, and high glucagon doses caused side effects like nausea. More research is needed to develop optimized glucagon-based obesity drugs.
Lower doses of glucagon combined with other hormones like GLP-1 show promise for long-term weight reduction with fewer side effects. However, large, high-quality clinical trials are still needed.
While glucagon’s weight loss potential is exciting, individuals should not use glucagon for this purpose until rigorous safety and efficacy data is available.
Glucagon Regulation
Glucagon regulation is a fundamental mechanism in the intricate balance of blood glucose levels, ensuring our body has a steady energy supply, especially during fasting or between meals.
The pancreas orchestrates This regulatory system, with alpha cells responsible for producing and releasing glucagon in response to low blood glucose levels, primarily serving as a signal to the liver to release stored glucose through glycogenolysis and stimulate gluconeogenesis.
In this dynamic interplay of hormones, glucagon acts as a counterbalance to insulin, preventing hypoglycemia by promoting the release of glucose into the bloodstream when needed most while also facilitating the breakdown of fat for energy.
| Aspect of Glucagon Regulation | Description |
|---|---|
| 1. Hormone Source | – Glucagon hormone is produced and released by the alpha cells of the pancreas, specifically in the islets of Langerhans. |
| 2. Stimulating Signals | – Low Blood Glucose Levels: The primary trigger for glucagon release is when blood glucose levels drop below a certain threshold. |
| – Sympathetic Nervous System: Activation of the sympathetic nervous system, often in response to stress or exercise, can also stimulate glucagon release. | |
| 3. Inhibitory Signals | – High Blood Glucose Levels: Elevated blood glucose levels, typically in response to a meal, inhibit glucagon release. |
| – Insulin: Insulin, produced by beta cells in the pancreas, counters the effects of glucagon. Increased insulin levels suppress glucagon release. | |
| 4. Target Organs and Effects | – Liver: Glucagon primarily targets the liver. It promotes glycogenolysis, the breakdown of glycogen into glucose, and gluconeogenesis, the synthesis of glucose from non-carbohydrate sources. |
| – Adipose Tissue: Glucagon enhances lipolysis, the breakdown of triglycerides into fatty acids, which are used for energy production. | |
| – Muscle: Glucagon has minimal direct effects on muscle tissue but indirectly influences glucose availability for muscle through its actions on the liver. | |
| 5. Physiological Role | – Blood Glucose Regulation: Glucagon plays a crucial role in maintaining blood glucose levels during fasting and between meals. |
| – Counterregulatory Hormone: It acts as a counterregulatory hormone to insulin, ensuring glucose availability when needed. | |
| 6. Regulatory Mechanisms | – Feedback Loop: Glucagon release is tightly regulated by a negative feedback loop. When blood glucose levels rise, insulin secretion increases, suppressing glucagon release. |
| – Coordinated Hormonal Response: Glucagon works in concert with other hormones like insulin and epinephrine to maintain glucose homeostasis. | |
| 7. Clinical Implications | – Diabetes: Dysregulation of glucagon can contribute to blood glucose dysregulation in diabetes. |
| – Therapeutic Target: Understanding glucagon regulation is crucial for developing treatments for diabetes and other metabolic disorders. |
Understanding the intricate regulation of glucagon is essential for comprehending glucose homeostasis, metabolic health, and managing conditions like diabetes.
How to Maintain Healthy Glucagon Levels
Here are some tips for optimizing your glucagon levels and glucose homeostasis:
- Eat regular, balanced meals. Avoid going too long without eating to prevent hypoglycemia from low glucagon hormone.
- Choose low-GI foods. Low-glycemic-index foods release glucose slowly, requiring less glucagon response.
- Manage stress. Chronic stress raises glucagon. Practice relaxation techniques.
- Exercise regularly. Physical activity improves insulin and glucagon sensitivity.
- Don’t smoke. Smoking stimulates alpha cells to release more glucagon.
- Limit alcohol. Excess alcohol can increase glucagon secretion.
- Maintain a healthy weight. Obesity is linked to dysregulated glucagon release.
- Take any medications as directed. Certain drugs, like insulin, can influence glucagon levels.
- See your doctor regularly – Your provider can check for potential issues with glucose control.
While individuals cannot directly control glucagon levels, a healthy lifestyle can help maintain ideal glucose homeostasis.
Hyperglycemic agent
Overdoses of insulin given to diabetic patients often result in acute hypoglycemia. It may be cured by giving crystalline glucagon (in the form of glucagon hydrochloride) intra-muscularly (or) intravenously. Response may be observed within 10 to 15 minutes after administration of 0.5 to 1.0 mg of glucagon.
Functions of Glucagon
- Glucagon stimulates glycogenolysis.
- Glucagon acts through cAMP as its second messenger.
- Glucagon stimulates gluconeogenesis by activation of pyruvate carboxylase.
- Glucagon inhibits glucose oxidation by inhibiting pyruvate kinase.
- It increases potassium release from the liver.
- In adipose tissue and the liver, it increases the breakdown of lipids into fatty acids and glycerol.
Frequently Asked Questions on Glucagon Hormone
What happens if glucagon levels are too high?
Excessively high glucagon levels can lead to hyperglycemia (high blood sugar). Chronically elevated glucagon is seen in some cases of uncontrolled diabetes. Very high glucagon can also increase ketone production and the risk of ketoacidosis.
What happens if glucagon levels are too low?
Low glucagon hormone levels or a reduced glucagon response can result in hypoglycemia (low blood sugar). It is most dangerous for people with diabetes who are dependent on insulin. Without enough glucagon, they cannot counteract insulin’s effects and raise blood glucose.
What diseases involve abnormal glucagon levels?
Diabetes (both type 1 and advanced type 2) often involves dysregulated glucagon release. Glucagonomas are rare pancreatic tumors that oversecrete glucagon, causing high blood sugar. Defects in the glucagon receptor can also alter glucagon signaling.
What are the most important glucagon effects?
The main effects of glucagon are:
– Increased glucose output from the liver
– Stimulating glycogen breakdown
– Gluconeogenesis: glucose production
– Elevated blood sugar levels
– Appetite suppression
– Increased lipolysis and fat oxidation
How can I check my glucagon levels?
There is no routine clinical test for directly measuring glucagon levels. However, blood glucose monitoring can detect dysregulation of glucagon’s effects. Your doctor may check glucagon and insulin levels if an abnormality in glucose homeostasis is suspected.
Conclusion
Glucagon is an essential metabolic hormone for blood sugar regulation between meals and fasting. It counterbalances insulin action by stimulating hepatic glucose release and preventing hypoglycemia.
Dysregulation of glucagon secretion or response underlies many cases of diabetes mellitus. Restoring normal glucagon biology represents an exciting area of diabetes research. Glucagon hormone may also have potential as a weight loss treatment.
Maintaining healthy glucagon levels through diet, exercise, stress management, and medication adherence can optimize glucose homeostasis long-term. Further research on glucagon hormone will uncover new aspects of its biology and lead to novel therapies for diabetes and obesity.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.


