Gastrointestinal hormones, or gut hormones, are a group of hormones secreted by enteroendocrine cells in the stomach, pancreas, and small intestine. These hormones play crucial roles in regulating various aspects of the digestive system and overall physiological processes.
The gastrointestinal tract is controlled by an intricate system of hormones secreted by specialized cells. These gastrointestinal hormones regulate digestive functions like gastric acid secretion, gastrointestinal motility, appetite, and glucose homeostasis. This article comprehensively overviews the major gastrointestinal hormones’ functions, regulation, and clinical significance.
The digestion and absorption of nutrients are complicated processes regulated by the automatic nervous system. It occurs in association with peptide hormones of the gastrointestinal tract (GIT).
The specialized cells lining the gastrointestinal tract are responsible for producing gastrointestinal hormones. Hence, the intestinal tract may be considered the most enormous mass of cells that secrete hormones. Many gastrointestinal hormones have been identified. However, only gastrointestinal tract hormones have been well characterized.
What is a gastrointestinal hormone?
Gastrointestinal hormones are hormones secreted by the gastrointestinal tract’s cells. They regulate various digestive functions and help maintain gastrointestinal health.
Gastrointestinal hormones, as endocrine hormones, wield significant influence over the digestive system, orchestrating a complex symphony of functions. Among these hormones, gastrin emerges as a critical player, its effects extending to the secretion of gastric acid, demonstrating the trophic effect of gastrin on the stomach. This trophic hormone plays a role in regulating growth and has direct implications for the gastric mucosa.
Definition of Gastrointestinal Hormones
- Gastrointestinal hormones are chemical messengers secreted by the endocrine cells of the digestive system.
- They are produced in response to food consumption and help regulate digestion, absorption, appetite, glucose metabolism, and gastrointestinal motility.
Importance of Gastrointestinal Hormones in Digestion
The intricate interactions between these gastrointestinal hormones, their shared trophic effects, and their collective influence on the digestive system underscore their importance in maintaining a healthy gastrointestinal tract.
Their functions, from regulating gastric acid secretion to the growth of gastrointestinal tissues, demonstrate their pivotal role in the delicate balance required for efficient digestion and overall health.
- Gastrointestinal hormones are vital in optimizing digestion and regulating appetite and food intake.
- They coordinate the activities of the digestive organs like the stomach, pancreas, liver, and gallbladder.
- Gastrointestinal hormones influence processes like:
- Gastric acid, pancreatic, and bile secretion
- Absorption of nutrients
- Gastrointestinal motility
- Appetite and satiety
- Glucose homeostasis
Overview of the Endocrine System in the Gastrointestinal Tract
- The gastrointestinal tract contains several types of endocrine cells that secrete hormones.
- The primary cell types include:
- Enteroendocrine cells: found along the intestinal mucosa
- G cells secrete gastrin.
- I cells secrete cholecystokinin.
- S cells: secrete secretin
- P/D cells secrete somatostatin
- L cells – Secrete PYY and GLP-1
- Together, these endocrine cells regulate various aspects of digestion through hormone secretion.
Different Types of Gastrointestinal Hormones and Their Functions
Various types of gastrointestinal hormones play crucial roles in several physiological processes.
- Gastrin is a hormone released by the stomach that stimulates the secretion of gastric acid, aiding in the digestion of food.
- Cholecystokinin (CCK) is produced in the small intestine, and it stimulates the release of digestive enzymes from the pancreas and the contraction of the gallbladder for efficient digestion.
- Secretin is another hormone produced by the small intestine, which stimulates the release of bicarbonate-rich pancreatic juice, helping neutralize stomach acid.
- Ghrelin, made in the stomach, stimulates appetite and promotes food intake. Leptin, on the other hand, is produced by adipose tissue and helps regulate appetite and metabolism.
- Somatostatin, made in various parts of the gastrointestinal tract, inhibits the release of several hormones. Motilin, produced by the small intestine, regulates gastrointestinal motility.
- Peptide YY (PYY) is made in the colon and small intestine, suppressing appetite and reducing food intake. These gastrointestinal hormones play diverse roles in digestion, metabolism, and appetite regulation.
Several critical gastrointestinal hormones help regulate digestive functions. The major ones are described below:
1. Gastrin
Gastrointestinal hormones are pivotal in regulating various physiological functions within the digestive system. Among these hormones, gastrin holds a prominent place, particularly in the context of gastric mucosal growth. It is known to have a trophic effect on the stomach, promoting the development of gastric mucosa.
Gastrin is an essential gastrointestinal hormone primarily involved in stimulating gastric acid secretion.
This trophic effect can be attributed to the role of gastrin in regulating the gastric inhibitory polypeptide, one of the well-known gastrointestinal hormones. In this intricate network of hormonal interplay, gastrin, along with other gastrointestinal hormones, influences the growth of the stomach and the upper gastrointestinal tract.
It regulates multiple aspects of gastric function, including secretion, motility, and growth.
Source and Secretion
- Gastrin is secreted by specialized enteroendocrine cells called G cells in the gastric antrum and duodenum.
- G cells occur mainly in the pyloric antrum of the stomach, with lower concentrations in the proximal small intestine.
Structure and Forms
- Gastrin is synthesized as a large precursor molecule called preprogastrin.
- It is cleaved to form progastrin, which is further processed to produce various active forms of gastrin:
- G17: 17 amino acid form
- G34: 34 amino acid form
- G71: 71 amino acid form
- G17 is the major circulating and biologically active form.
Functions
Gastrin has several essential functions:
- Stimulates gastric acid secretion: Gastrin is the most potent stimulator of gastric acid release from parietal cells. It helps create an acidic environment needed for protein digestion and absorbing nutrients like calcium, iron, and vitamin B12.
- Increases gastric motility: Gastrin increases muscular contractions in the antrum and duodenum. It helps grind up food and propel it forward.
- Promotes growth of gastric mucosa – Gastrin causes the proliferation of cells lining the stomach, including acid-producing parietal and mucus-secreting cells. It increases the functional capacity of the stomach.
- Parietal cell growth and differentiation: Gastrin induces the maturation of parietal cell precursor cells into mature acid-secreting parietal cells. It amplifies the ability to secrete gastric acid.
- Pancreatic secretion may enhance the secretion of enzymes and bicarbonate from the pancreas.
Regulation of Release
Neural, hormonal, and chemical factors control gastrin release:
- Vagal nerve stimulation – Acetylcholine released by the vagus nerve enhances gastrin secretion.
- Gastric distension: stretching of stomach walls triggers gastrin release.
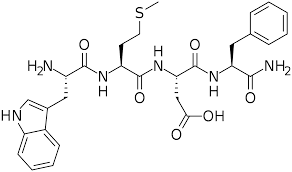
- Amino acids – The presence of amino acids in the stomach, especially phenylalanine, stimulates gastrin secretion.
- Calcium: Extracellular calcium stimulates gastrin release.
- Gastric acidity – Acidic gastric contents inhibit gastrin release due to a negative feedback mechanism.
- Somatostatin – The release of somatostatin by delta cells in the stomach suppresses gastrin secretion.
Pathophysiology
Abnormalities in gastrin secretion or activity can lead to:
- Hypergastrinemia – Excess gastrin is seen in conditions like pernicious anemia, antral G cell hyperplasia, gastrinomas, atrophic gastritis, and renal failure. It can cause peptic ulcer disease.
- Hypogastrinemia – Insufficient gastrin, which occurs after gastrectomy, reduces acid secretion.
- Gastrinomas – Gastrin-secreting tumors result in high gastrin levels and multiple peptic ulcers, known as Zollinger-Ellison syndrome.
Clinical Uses
- Diagnosis of pernicious anemia: High gastrin levels indicate atrophic gastritis and vitamin B12 deficiency.
- Gastric acid analysis – Serum gastrin levels and gastric pH help assess hypochlorhydria or achlorhydria.
- Stress ulcer prevention: Gastrin receptor antagonists may be prophylactically given to critically ill patients to reduce stress-induced ulceration.
The role of gastrointestinal hormones goes beyond their functions. It encompasses their ability to impact gastric and duodenal mucosa growth, exemplifying their multifaceted effects within the gastrointestinal system.
Gastrin, expressed through the gastrin gene, is in this intricate network of hormonal interplay. It shares this stage with various other gastrointestinal hormones, collectively contributing to regulating growth and maintaining the digestive system.
In summary, gastrin is an essential GI hormone that controls multiple aspects of gastric physiology. Its secretion is tightly regulated, and abnormalities can lead to disorders like ulcer disease and hypersecretion. Gastrin testing has diagnostic utility in medicine.
2. Cholecystokinin (CCK)
Cholecystokinin is a hormone produced by the small intestine that regulates multiple digestive functions, including enzyme secretion, gallbladder contraction, and satiety.
The release of gastrointestinal hormones, including gastrin and cholecystokinin (CCK), is tightly regulated and orchestrated to maintain the delicate balance required for efficient digestion. These hormones are secreted by specialized cells in the gastrointestinal tract and pancreas.
In addition to their role in regulating growth, gastrointestinal hormones, including gastrin and others, have also been identified as incretin hormones.
These hormones may enhance the effects of other hormones, such as insulin, affecting glucose homeostasis. Such interplay between hormones within the human gastrointestinal mucosa highlights the intricate nature of gastrointestinal endocrinology.
They profoundly impact the release of trophic hormones and play a role in inhibiting other trophic hormones, demonstrating the complexity of their regulatory functions.
Source and Secretion
- CCK is secreted by enteroendocrine I cells in the mucosal epithelia of the duodenum and jejunum.
- It is synthesized from proCCK as a more significant inactive precursor and then enzymatically cleaved into active forms like CCK-58, CCK-33, CCK-22, and CCK-8.
- CCK-33 and CCK-8 are the primary bioactive forms.
Release Stimuli
- The presence of proteins and fats, especially fatty acids, in the duodenum strongly stimulates CCK release.
- Gastric distension and vagal nerve stimulation also enhance CCK secretion.
- Bile salts may amplify CCK release.
Functions
- Stimulates pancreatic enzyme secretion: CCK stimulates acinar cells of the pancreas to secrete digestive enzymes like trypsin, chymotrypsin, amylase, and lipase. It facilitates digestion.
- Contracts gallbladder: CCK induces gallbladder contraction and relaxation of the sphincter of Oddi, causing bile release into the duodenum. It aids fat digestion.
- Delays gastric emptying: CCK decreases the stomach’s motility to slow gastric emptying and increase food retention time.
- Induces satiety: By acting on CCK receptors in the nervous system, CCK promotes a feeling of fullness after eating, thus regulating food intake.
Regulation
- Somatostatin inhibits CCK secretion by acting on delta cells.
- Tryptophan reduces CCK release via negative feedback after protein digestion.
- Neural signals and hormones like leptin and ghrelin also modulate CCK release.
Clinical Relevance
- CCK receptor agonists may help manage appetite and obesity.
- CCK-based imaging agents can assess gallbladder ejection fraction.
- CCK antagonists are being studied for irritable bowel syndrome treatment.
CCK is an essential gastrointestinal hormone that facilitates digestion and appetite control through its actions on the pancreas, gallbladder, stomach, and nervous system.
Overall, the significance of gut hormones in gastrointestinal function cannot be overstated. These hormones, including gastrin and CCK, play a crucial role in releasing gastrointestinal hormones, influencing trophic hormones and demonstrating their importance in the growth and regulation of the digestive system.
Their far-reaching effects on the gastrointestinal tract and pancreas underscore their importance in maintaining the delicate balance required for efficient digestion and overall health.
3. Secretin
Secretin is a hormone produced by the small intestine that regulates pancreatic secretion, gastric acid release, and bile flow.
Source and Secretion
- Secretin is secreted by specialized enteroendocrine S cells located in the mucosa of the duodenum.
- Release is stimulated by gastric acid entering the duodenum and the presence of fatty acids in the duodenal lumen.
- Low duodenal pH caused by acid is the strongest trigger for secretin secretion.
Structure
- Secretin is initially synthesized as a 120-amino acid precursor, prosecretin.
- It is cleaved into the active 27-amino acid polypeptide secretin.
Functions
- Stimulates pancreatic bicarbonate secretion – Secretin acts on pancreatic ductal cells, causing a release of bicarbonate-rich alkaline fluid. It neutralizes the acidic chyme entering from the stomach.
- Inhibits gastric acid secretion: By increasing bicarbonate and pancreatic fluid secretion, secretin reduces further gastric acid release via a negative feedback mechanism.
- Stimulates bile flow: Secretin enhances bile production by the liver and its release from the gallbladder into the duodenum.
- Slightly delays gastric emptying. It may slow down gastric motility modestly to increase nutrient absorption time.
Regulation
- Somatostatin inhibits secretin release.
- Secretin secretion is reduced when duodenal pH rises due to negative feedback.
- CCK and secretin stimulate each other’s release.
- Neural signals and other hormones like leptin modulate secretin secretion.
Clinical Uses
- A secretin stimulation test assesses pancreatic function in patients suspected of chronic pancreatitis.
- Synthetic secretin is used in endoscopy to improve visualization by increasing pancreatic secretions.
- They were studied for potential use in treating autism gastrointestinal symptoms.
- Secretin is key in optimal digestion by coordinating pancreatic and gastric secretions and regulating bile flow.
4. Ghrelin
Ghrelin is a peptide hormone produced mainly by the stomach that strongly stimulates appetite and food intake.
Source and Secretion
- Ghrelin is predominantly synthesized and secreted by X/A-like cells within the oxyntic glands of the gastric fundus.
- Smaller amounts are produced in the pancreas, intestine, hypothalamus, and other tissues.
Structure and Forms
- Ghrelin is derived from a 117 amino acid preproghrelin precursor.
- The active form is a 28 amino acid peptide with an octanoyl fatty acid side chain.
- Acylation by ghrelin O-acyltransferase (GOAT) enzyme is essential for its biological activity.
Release Stimuli
- Circulating ghrelin levels rise during fasting and drop rapidly after a meal.
- Weight loss, insulin, leptin, and sympathetic nervous activity enhance ghrelin secretion.
- Somatostatin, obesity, and high glucose inhibit its release.
Functions
- Stimulates appetite and food intake – Ghrelin activates neurons in the hypothalamus and brainstem that promote hunger and meal initiation. It leads to increased food consumption.
- Adiposity – By enhancing appetite, ghrelin promotes fat deposition and higher body weight.
- Increases gastric motility and acid – Ghrelin contracts the stomach musculature and stimulates acid secretion. It accelerates digestion.
- Glucose metabolism – Counteracts insulin to raise blood glucose levels. It may play a role in glucose homeostasis.
Clinical Relevance
- Ghrelin receptor antagonists are being developed as anti-obesity drugs.
- Ghrelin levels are reduced in obesity and elevated in anorexia nervosa.
- Ghrelin administration may help with cachexia (wasting) associated with cancer, kidney failure, etc.
In summary, the hunger hormone ghrelin is a crucial driver of food intake and weight gain by activating appetite stimulation pathways in the brain and stomach.
5. Leptin
Leptin is a hormone secreted by adipose tissue that suppresses appetite and regulates long-term energy balance.
Source and Secretion
- Leptin is predominantly synthesized and secreted by white adipose tissue.
- The placenta, mammary epithelium, skeletal muscle, stomach, and other tissues also produce smaller amounts.
Release Stimuli
- Fat mass and adipocyte size are the main determinants of leptin levels.
- Overfeeding, insulin, glucocorticoids, and inflammatory mediators stimulate leptin secretion.
- Fasting, testosterone, and growth hormone inhibit its release.
Mechanism of Action
- Leptin binds to and activates specific leptin receptors in the hypothalamus.
- It inhibits orexigenic neurons that stimulate appetite.
- Leptin also activates anorexigenic neurons that suppress appetite.
- Ultimately, leptin reduces food intake and increases energy expenditure.
Functions
- Suppresses appetite – Leptin acts on the hypothalamus to diminish hunger and promote satiety.
- Reduces food intake – By suppressing appetite, leptin decreases overall food consumption and portion sizes.
- Increases energy expenditure – Leptin elevates fat oxidation rates and thermogenesis.
- Regulates long-term energy balance – Leptin levels proportional to fat mass maintain equilibrium between energy intake and expenditure.
Clinical Relevance
- Leptin deficiency causes severe obesity, highlighting its key role in weight regulation.
- Increased leptin levels in obesity fail to suppress appetite due to leptin resistance.
- Recombinant leptin therapy can treat rare leptin deficiency states.
- Leptin is being explored as a potential obesity pharmacotherapy.
In summary, the adipose-derived hormone leptin controls food intake, metabolism, and body weight over the long term.
Other Gastrointestinal Hormones
In addition to the major hormones, several other gastrointestinal hormones play regulatory roles:
6. Somatostatin
Somatostatin is a peptide hormone that inhibits the secretion of several other gastrointestinal hormones. It helps regulate digestive processes.
Source and Secretion
- Somatostatin is secreted by specialized delta cells (also called D cells) located in the:
- Stomach
- Pancreas
- Duodenum
- Jejunum
- Also known as growth hormone-inhibiting hormone (GHIH)
Structure
- Initially synthesized as a 92 amino acid preprosomatostatin precursor
- Cleaved to form pro somatostatin
- Further processed to produce:
- Somatostatin-14 (SS-14) – 14 amino acid active form
- Somatostatin-28 (SS-28) – 28 amino acid active form
Release Stimuli
- Presence of nutrients in the gut lumen
- Low pH/luminal acidification
- Neural stimulation by the sympathetic nervous system
- Amino acids, especially tryptophan
Functions
- Inhibits secretion of multiple gastrointestinal hormones:
- Gastrin
- Secretin
- Cholecystokinin
- Motilin
- Vasoactive intestinal peptide
- Reduces gut motility and smooth muscle contractions
- Decreases gastric acid, pepsin, and bile secretion
- Lowers pancreatic enzyme production
- Suppresses release of insulin and glucagon
Clinical Uses
- Octreotide and other somatostatin analogs treat acromegaly, diarrhea, ulcers, fistulas, bleeding varices, and other conditions involving excessive gut secretions.
In summary, somatostatin is a crucial inhibitory hormone that regulates digestive secretions and motility by suppressing other gastrointestinal hormones.
7. Motilin
Motilin is a crucial hormone that regulates gastrointestinal motility patterns and stimulates gastric emptying.
Source and Secretion
- Motilin is secreted by specialized enteroendocrine Mo cells in the duodenum and jejunum.
- The highest concentrations are found in the proximal small intestine.
Structure
- Synthesized as an inactive 112 amino acid preprohormone.
- It is cleaved into the 22 amino acid active polypeptide motilin.
Release Stimuli
- Fasting – motilin levels peak during the inner digestive phase.
- Gastric acid – luminal acidity stimulates motilin release.
- The presence of fat in the duodenum enhances secretion.
- Neural cholinergic input activates Mo cells.
Functions
- It initiates phase III contractions of the migrating motor complex.
- Stimulates muscular peristaltic contractions to sweep undigested material through the GI tract.
- It accelerates gastric emptying.
- It increases lower esophageal sphincter pressure.
- It stimulates pepsin secretion.
Regulation
Release is inhibited by:
- Feeding: nutrient detection suppresses motilin
- Somatostatin
- High intestinal osmolality
- Neural signals and gastrointestinal hormones like ghrelin modulate motilin secretion.
Clinical Relevance
- Motilin analogs like camicin are being developed to treat gastroparesis, reflux, and other motility disorders.
- Plasma motilin was measured to assess gastroparesis.
The gastrointestinal hormone motilin is critical for generating migrating motor complexes and optimizing gut motility patterns.
8. Peptide YY (PYY)
Peptide YY (PYY) is a hormone secreted by the gastrointestinal tract that reduces appetite and decreases food intake.
Source and Secretion
- PYY is produced and secreted by enteroendocrine L cells in the distal gut, primarily the ileum, colon, and rectum.
- The highest concentrations were in the rectum, sigmoid colon, and ileum.
Structure
- Synthesized as a 97-amino acid preproPYY protein.
- Enzymatically cleaved into:
- PYY1-36 – 36 amino acid active form
- PYY3-36 – 34 amino acid primary circulating form
Release Stimuli
- Nutrient intake – feeding stimulates PYY release proportional to caloric load.
- Presence of nutrients in the ileum, especially fat and bile acids.
- Neural and endocrine factors like insulin, leptin, cholecystokinin.
Mechanism of Action
- PYY3-36 acts on Y2 receptors of arcuate nucleus neurons in the hypothalamus.
- Inhibits orexigenic NPY neurons to suppress appetite.
- It may also act via vagal afferent neurons.
Functions
- The powerful appetite suppressant increases satiety.
- Decreases food intake and reduces meal size.
- Delays gastric emptying to induce fullness.
- It suppresses pancreatic exocrine secretion.
Clinical Relevance
- Low PYY levels associated with obesity – fails to suppress appetite sufficiently.
- PYY administration decreases hunger and food intake in both lean and obese subjects.
- Potential target for anti-obesity drugs.
In summary, PYY is an essential gut hormone that regulates appetite and digestion through its actions on the hypothalamus, stomach, pancreas, and other organs.
Regulation of Gastrointestinal Hormones
These hormones are released by specialized cells scattered throughout the gastrointestinal tract, including enteroendocrine cells and other sites, each with its unique expression of the gastrointestinal hormone. The effects of gastrin, for instance, encompass the regulation of gastric acid secretion and its influence on other trophic hormones. This interaction within the digestive system highlights the entwined nature of gastrointestinal hormonal regulation.
The secretion of gastrointestinal hormones is tightly regulated by various mechanisms:
a. Neural Regulation
- The autonomic nervous system regulates hormone secretion through:
- Vagal stimulation
- Sympathetic stimulation
b. Feedback Mechanisms
- Hormones inhibit or stimulate the secretion of other hormones through feedback loops. Examples:
- Somatostatin inhibits several GI hormones
- Secretin and CCK stimulate each other’s release
c. Hormonal Regulation
- Non-GI hormones like leptin, ghrelin, and insulin modulate the release of GI hormones.
d. Nutrient and Digestive Product Sensing
- Nutrients like fatty acids and amino acids in the gut lumen trigger hormone release.
- Gastric acidity and luminal pH influence hormone secretion.
Clinical Implications
Furthermore, gastrointestinal peptides and their role in the trophic hormone of the stomach add another layer of complexity to the intricate world of gastrointestinal hormones. The effects of gastrin are intertwined with the actions of these peptides, demonstrating the integrated functioning of these hormones.
They are not merely isolated players but are connected, shaping the growth of the gastric and duodenal mucosal tissues and contributing to the broader field of gastrointestinal hormones and gut health.
Gastrointestinal hormones have several critical clinical associations:
a. Gastrointestinal Hormone Disorders
- Hypergastrinemia: Excess gastrin production leads to peptic ulcer disease.
- Nesidioblastosis – Hyperinsulinemic hypoglycemia caused by excess incretins like GLP-1.
- Post-gastrectomy dumping syndrome – Rapid gastric emptying due to lack of pyloric sphincter.
b. Therapeutic Uses of Gastrointestinal Hormones
- Octreotide (somatostatin analog) reduces GI secretions in diarrhea and ulcers.
- GLP-1 receptor agonists like exenatide are used to treat diabetes due to their incretin effects.
c. Obesity and Gastrointestinal Hormones
- Altered GI hormone profiles influence appetite regulation and glucose homeostasis in obesity.
- Bariatric surgery changes GI hormone levels to promote weight loss.
- Ghrelin has emerged as a potential target for anti-obesity drugs.
Frequently Asked Questions (FAQs) on Gastrointestinal Hormones
What are the main functions of gastrin?
Gastrin is secreted by G cells in the stomach and duodenum. Its main functions are stimulating gastric acid secretion, enhancing gastric motility, increasing the growth of gastric mucosa, and promoting parietal cell growth and differentiation.
How does cholecystokinin regulate digestion?
Cholecystokinin (CCK) is secreted by I cells in the small intestine. It stimulates pancreatic enzyme secretion, causes gallbladder contraction, inhibits gastric emptying, and induces satiety – all of which facilitate digestion and appetite control.
What stimulates the release of secretin?
Secretin release is stimulated by gastric acid in the duodenum and fatty acids. The drop in duodenal pH caused by gastric acid triggers secretin secretion, inhibiting further gastric acid secretion and thus forming a negative feedback loop.
Where is ghrelin produced, and how does it impact appetite?
The stomach predominantly produces ghrelin. It stimulates appetite and food intake while also promoting adiposity and weight gain. Ghrelin levels rise during fasting and fall after meals, influencing hunger signals.
What is the role of somatostatin in regulating gastrointestinal hormones?
Somatostatin is an inhibitory hormone released by delta cells in the GI tract. It inhibits the secretion of several other hormones like gastrin, secretin, CCK, and motilin. It helps turn off digestive secretions when nutrients have been absorbed.
Conclusion
Summary of Key Points
- Gastrointestinal hormones like gastrin, CCK, and secretin regulate digestive functions.
- They are secreted by specialized Enteroendocrine cells – lining the gut mucosa.
- Their release is tightly controlled by neural signals, nutrient sensing, pH changes, and feedback loops.
- Dysregulation of GI hormones is implicated in disorders like ulcers, diarrhea, diabetes, and obesity.
Significance of Gastrointestinal Hormones in Digestive Health
The physiological significance of gut hormones extends beyond their role in gastric and duodenal mucosal growth. These hormones have been shown to affect the entire gastrointestinal tract, influencing processes like gastric and duodenal mucosal hyperplasia. It’s essential to understand that the effects of gut hormones go beyond the confines of the stomach; they have far-reaching implications for the entire digestive system.
Gastrointestinal hormones form an integral network that controls appetite, digestion, absorption, and metabolism. Understanding the complex interplay between these hormones provides insight into maintaining gastrointestinal health and developing therapeutic approaches to digestive and metabolic disorders.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.