Insulin is a crucial hormone that helps regulate blood sugar levels in the body. With the increasing rates of diabetes, especially type 2 diabetes, understanding this pancreatic hormone, how it works, and the different types available is important for managing this disease. This article provides an in-depth look on the role of insulin and to maintaining healthy blood glucose levels.
Insulin is a hormone produced by the pancreas that plays an essential role in regulating blood sugar levels and enabling the body to process glucose for energy. Maintaining healthy insulin levels is critical for overall health and wellbeing.
When the body does not produce enough insulin or becomes resistant to its effects, blood sugar can spike, leading to hyperglycemia. On the other hand, excessive insulin can cause blood sugar to drop dangerously low, resulting in hypoglycemia. Understanding how this Blood sugar controller works is key for properly managing diabetes and related metabolic disorders.
In this comprehensive guide, we will explore the discovery, structure, function, and regulation of insulin. We will also discuss the different types of diabetes, methods of administering insulin therapy, and the impact of lifestyle factors. With the latest advances in technology, research and innovation are continuously improving the management and treatment options for diabetes.
The Discovery of Insulin
Historical Background
Throughout history, diabetes was a feared disease with no cure, often called the “wasting disease” since it caused severe weight loss. In the early 20th century, people with type 1 diabetes rarely lived more than a year or two after diagnosis.
That changed in 1921 when insulin was discovered by Dr. Frederick Banting and Charles Best in Canada. Working with biochemist James Collip and supervised by professor John Macleod, they successfully isolated insulin from the pancreas of dogs.
On January 11, 1922, they first administered the extract to 14-year-old Leonard Thompson, who was dying from diabetes. His blood sugar levels quickly stabilized, proving the extract contained the much-sought-after antidiabetic hormone. For this groundbreaking work, Banting and Macleod received the 1923 Nobel Prize in Medicine.
Impact on Diabetes Treatment

The discovery of insulin transformed type 1 diabetes from a deadly disease to a manageable condition. For the first time, people could regulate their blood sugar with daily insulin injections and control their symptoms.
Pharmaceutical companies rapidly produced and distributed insulin on a large scale. The first commercial insulin was marketed in 1923 as Iletin by Eli Lilly and Company. Over the next decades, This glycemic regulator purification and modifications led to human insulin by the 1970s and later analog insulins. The American Diabetes Association (ADA) characterizes insulin by how fast it works.
Today, insulin is considered one of the safest and most effective medications. With timely diagnosis and access to insulin, people with type 1 diabetes can live long healthy lives. The discovery of this Sugar-regulating hormone was a true medical breakthrough that saved millions of lives.
Milestones in Insulin-Related Research
Here are some key milestones in the history of insulin following its discovery:
- 1936: The amino acid structure of insulin was characterized.
- 1955: The first successful production of synthetic “human” insulin.
- 1978: Genentech produced the first biosynthetic “human” insulin using recombinant DNA technology.
- 1996: The US FDA approved the first insulin analog, insulin lispro (Humalog).
- 2004: The first inhaled insulin (Exubera) was introduced.
- 2006: The first insulin pump integrated with a continuous glucose monitor was approved.
- 2015: The first biosimilar insulin glargine (Basaglar) was approved.
- 2018: The first glucose-responsive “smart” insulin received FDA breakthrough status.
Researchers continue to build upon the pioneering discovery of insulin, improving diabetes care through both incremental innovations and game-changing breakthroughs.
What is Insulin and What Does it Do?

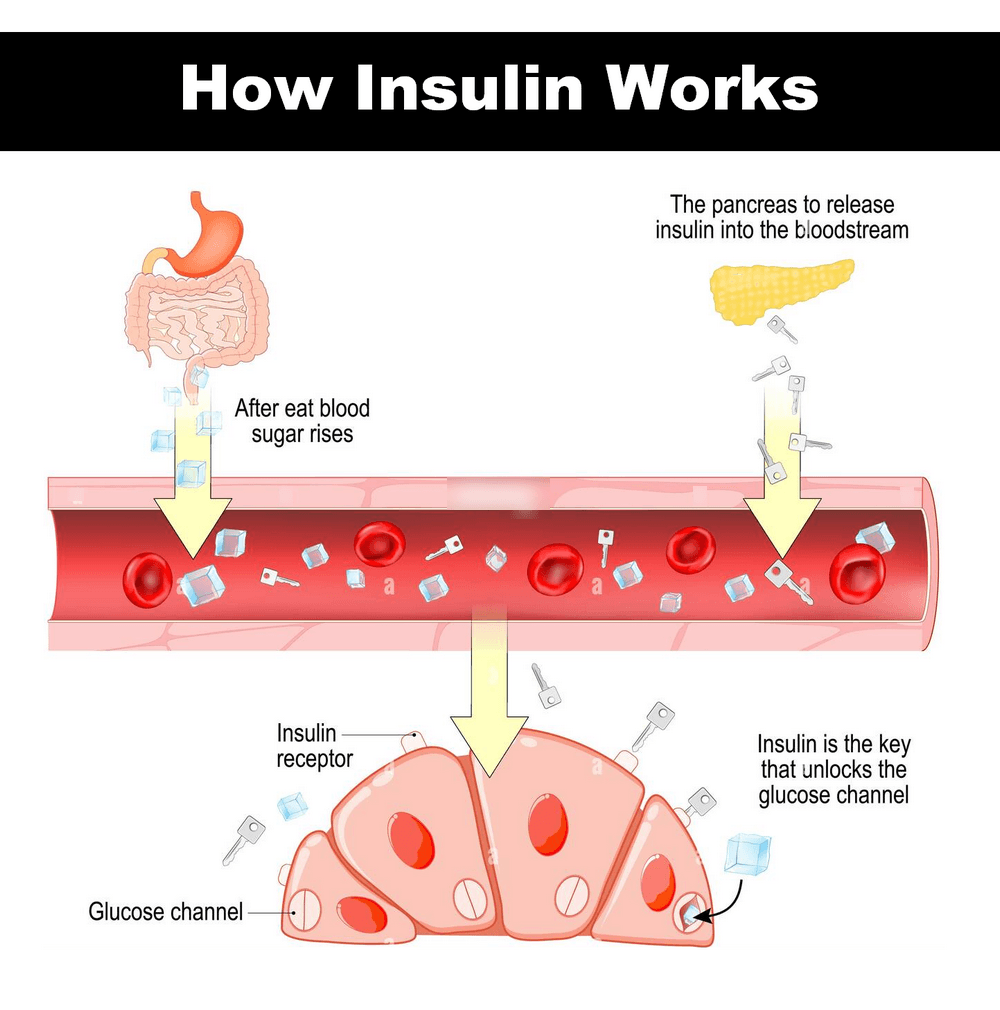
Insulin is a hormone produced in the pancreas by beta cells found in the islets of Langerhans. When we eat foods containing carbohydrates, our blood sugar (glucose) levels rise. This signals the pancreas to release insulin into the bloodstream. Insulin allows glucose to move from the blood into the body’s cells, where it can be used for energy.
Without enough insulin, blood sugar builds up in the bloodstream instead of being absorbed by the cells. Over time, high blood sugar levels can lead to serious medical complications like nerve damage, kidney disease, vision loss, heart disease, and stroke. People with diabetes either don’t produce enough insulin or are resistant to its effects. The length of time before insulin begins to take effect can vary depending on the type of insulin used and individual factors.
Structure and Function of Insulin
a. Molecular Structure
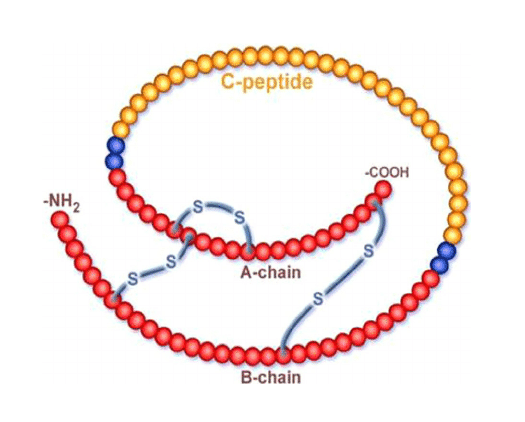
Insulin is a small protein hormone comprising two chains – an A chain with 21 amino acids and a B chain with 30 amino acids. It is formed and stored in the pancreas as a hexamer containing 6 insulin molecules bound together.
When released into the bloodstream, the hexamer dissociates into individual insulin molecules, called monomers. The monomeric form of insulin allows insulin to bind to target receptors and exert its effects in the body.
- In 1926, “ABEL” isolated crystalline insulin from pancreas.
- Insulin (insulaL =island) was first isolated in 1922 for the pancreas of dogs by Banting & Best of the university of Toranto , canada.
- It is the first hormone to be recognized as a protein. This is a Peptide hormone.
- The chemical structure of insulin has been determined by “Sanger” and his coworkers at Cambridge, England.
- The hormone consists of 51 amino acid residues dispersed in two chains.
- It contains two chains, they are A-chain & B-chain linked by disulfide bridges. A-chain contains 21 amino acids & B-chain contains 30 amino acid residues (molecular weight 5,733).
- Two Zinc atoms are always found with this hormone but is not a part of the insulin molecule. The main function of this two Zn+2 is, it stabilizes the hormonal structure.
- The position of disulfide bridges in the molecule,
| A-Chain | B-Chain | |
| Inter-disulphide bridges position | 7th Cys 20th Cys | 7th Cys 19th Cys |
| Intra-disulphide bridges position | 6-11th Cys | NIL |
b. Mechanism of Action
The hormone molecule acts by binding to a plasma membrane receptor on the target cells. Human insulin receptor gene is located on chromosome 19. In obesity, the number of receptors is decreases and target tissue becomes less sensitive to insulin. Insulin receptor (IR) is a glycoprotein with four subunits; two alpha and two beta subunits. The alpha units (135kD) are located on the beta subunits. The alpha units (135kD) are located on the extracellular side, to which insulin binds. The beta sub units (95kD) transverse the membrane and are exposed on the cytoplasmic side. Beta sub unit has tyrosine kinase activity.
Signal transduction: Binding of hormone causes dimerisation of the receptor. It is then internalized, so that the signal is transmitted. Then the tyrosine kinase phosphorylates tyrosine residues on the cytoplasmic side of insulin receptor. This event, in turn, phosphorylates insulin receptor substrates (IRS). IRS-1 and 2 are characterized. The message is later transmitted into a series of serine/threonine kinases. The final effect may be any one of the 3 following:
a) Gene transcription: Insulin acts at the transcription level to regulate synthesis of more than 100 proteins. This is effected through IR-2. For example; the following enzymes are induced by insulin: glucokinase, pyruvate kinase, phosphofructokinase, PFK-2, citrate cleavage enzyme, acetyl-coA carboxylase. Insulin represses the following enzymes: Glc-6-Phosphatase, PEPCK, Fru-1,6-bisphosphatase. Further the pathway through IRS-2 activates eIF-4E (eukaryotic Initiation Factor), so that protein synthesis is enhanced.
b) Activation of enzymes: The Hormone activates the exiting molecules of enzymes by covalent modification (phosphorylation or dephosphorylation). There are more than 50 enzymes activated by this mechanism.
c) DNA synthesis: Through the IRS-1 pathway, the hormone increases DNA synthesis, cell growth and anabolism.
In all above-mentioned pathways, intracellular mediators have been implicated in the hormonal action. There are Ca+2 and cAMP. Insulin activates phosphodiesterase and thereby decreases cAMP. So, reactions dependent on cAMP are inhibited, e.g.: glycogen phosphorylase.
The primary action of insulin is to control blood glucose levels by enabling cells throughout the body, especially muscle and fat cells, to take up excess glucose from the blood for energy or storage.
It binds to insulin receptors on cell surfaces, triggering a signaling cascade that results in the movement of glucose transporter proteins to the cell membrane. This facilitates the uptake of glucose into the cells.
Insulin also regulates the production and storage of fat, inhibits the breakdown of lipids, stimulates protein synthesis, and controls various metabolic pathways related to carbohydrate, fat, and protein metabolism.
c. Other Physiological Roles
In addition to its metabolic functions, insulin has several anabolic (growth-promoting) effects:
- Stimulates cell growth and differentiation
- Increases amino acid uptake into cells
- Promotes fat storage through lipogenesis
- Inhibits protein catabolism in muscle
- Modulates electrolyte balance
- Has vasodilatory effects to increase blood flow
- Involved in learning, memory, and neuronal survival
Therefore, insulin has widespread systemic effects that go beyond glucose homeostasis and are important for health.
What Are the Different Types of Insulin?
There are several types of insulin, each with its own characteristics in terms of onset, peak, and duration of action.
| Type | Name | Onset | Peak | Duration |
|---|---|---|---|---|
| Rapid-acting | NovoLog, Humalog, Apidra | 5-15 min | 30-120 min | ~3-5 hours |
| Short-acting (Regular/R) | U100: Humulin-R, Novolin-R | 30 min | 2-4 hours | 5-8 hours |
| Short-acting (Regular/R) | U-500: Humulin R U-500 | 30 min | 4-8 hours | 14-15 hours |
| Intermediate-acting (NPH) | Humulin N, Novolin N | 2-4 hours | 4-10 hours | 10-18 hours |
| Intermediate-acting (NPH) | Levemin | 1-3 hours | No peak | 18-24 hours |
| Long-acting | Lantus | 2-4 hours | No peak | 18-20 hours |
| Long-acting | Toujeo | 2-4 hours | No peak | 20-24 hours |
Here is a brief overview of the main types of insulin:
- Rapid-acting insulin: Begins working within 15 minutes, peaks in about 1 hour, and lasts for 2 to 4 hours. Examples are insulin lispro (Humalog), insulin as part (Novolog), and insulin glulisine (Apidra).
- Short-acting insulin: Starts working within 30 minutes, peaks anywhere from 2 to 3 hours, and is effective for 3 to 6 hours. Regular or R insulin falls in this category.
- Intermediate-acting insulin: Takes effect in 1 to 2 hours, peaks 4 to 12 hours later, and lasts for about 16 to 24 hours. NPH (Neutral Protamine Hagedorn) insulin is an intermediate-acting type.
- Long-acting insulin: Takes several hours to begin working, with little or no peak, and can last up to 24 hours. Examples include insulin detemir (Levemir) and insulin glargine (Lantus).
- Pre-mixed insulin: Contains fixed combinations of shorter-acting insulins (regular, lispro, aspart) and intermediate insulins (NPH) in one vial or pen.
The different types allow various options for matching the insulin profile to an individual’s needs and lifestyle for optimal blood sugar control. Rapid-acting insulin is given with meals while longer-acting insulins provide basal coverage. Rapid- or short-acting insulin is typically administered just before a meal to help manage blood sugar spikes after eating.
Regulation of Blood Sugar
Insulin Production and Secretion
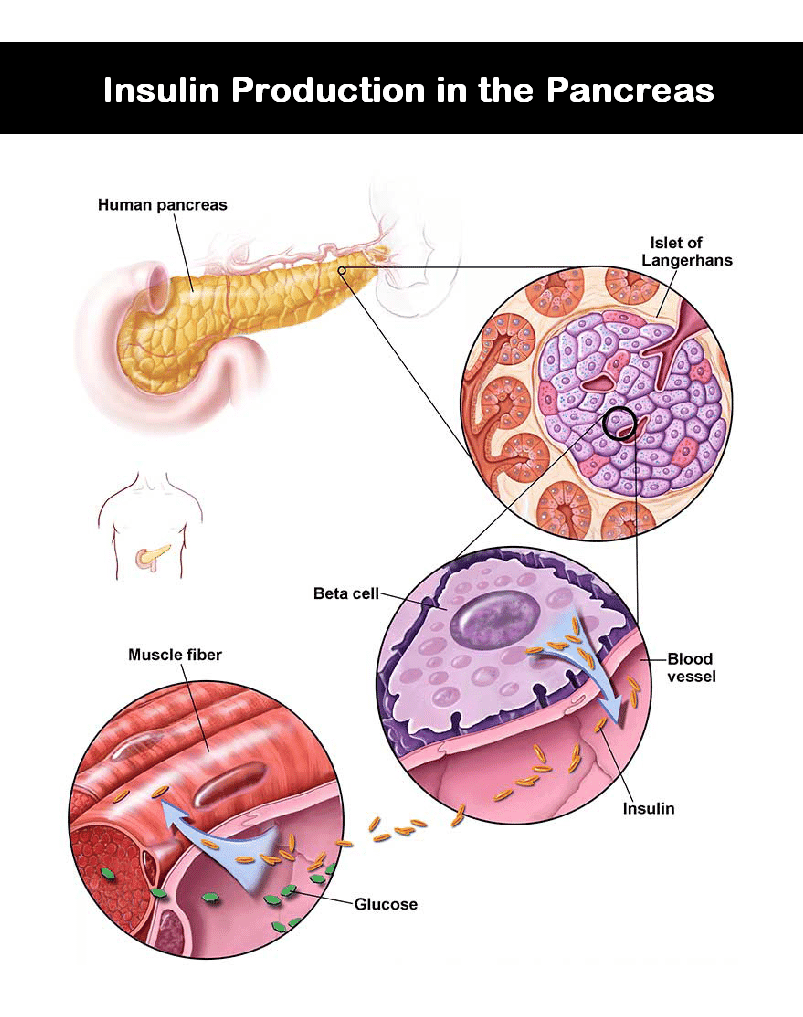
Insulin is synthesized and secreted by pancreatic beta cells found in clusters called the islets of Langerhans. Its release is tightly regulated to maintain normal blood glucose levels.
Glucose is the primary stimulus for insulin secretion. As blood glucose rises after a meal, increased glucose uptake by beta cells triggers insulin synthesis and secretion. Insulin is then released into the portal vein to signal the liver and other tissues to remove excess glucose from the bloodstream.
Insulin release occurs in a pulsatile manner, with oscillations every 6 to 15 minutes. There is also an ultradian rhythm of larger amplitude insulin secretions every 80 to 150 minutes.
Glucose Uptake and Utilization
Circulating insulin enables glucose uptake and utilization by insulin-sensitive tissues:
- Muscle: Insulin stimulates glucose uptake and glycogen synthesis. Muscle accounts for approximately 75% of whole body insulin-mediated glucose uptake.
- Adipose tissue: Insulin increases glucose uptake and conversion to triglycerides via lipogenesis.
- Liver: Insulin inhibits glucose production (gluconeogenesis) and stimulates glycogen synthesis for glucose storage.
This coordinated response promotes the efficient utilization and storage of glucose following meals.
Counterregulatory Hormones
Insulin release is balanced by counterregulatory hormones that have opposing effects:
- Glucagon: Secreted by pancreatic alpha cells, glucagon raises blood glucose levels by stimulating glycogenolysis and gluconeogenesis.
- Growth hormone: Antagonizes insulin by promoting lipolysis and insulin resistance.
- Cortisol: Increases gluconeogenesis and insulin resistance.
- Epinephrine: Stimulates glycogenolysis and gluconeogenesis.
These hormones counter the hypoglycemic effects of insulin and help maintain normal glucose homeostasis.
Types of Diabetes
Abnormalities in insulin production or function lead to diabetes mellitus. The main types include:
a. Type 1 Diabetes
In type 1 diabetes, pancreatic beta cells are destroyed by an autoimmune attack, resulting in insufficient insulin production. Without exogenous insulin administration, type 1 diabetes is fatal.
Onset is usually in childhood and adolescence, but can occur at any age. It accounts for 5-10% of diabetes cases. Risk factors include genetics and environmental triggers like viruses.
b. Type 2 Diabetes
Type 2 diabetes mellitus involves insulin resistance – cells fail to adequately respond to insulin, necessitating higher levels to maintain normal glucose metabolism. It begins with insulin resistance, and progresses to beta cell decline unable to compensate for increased demands. People with type 2 diabetes make insulin, but their bodies don’t respond well to it.
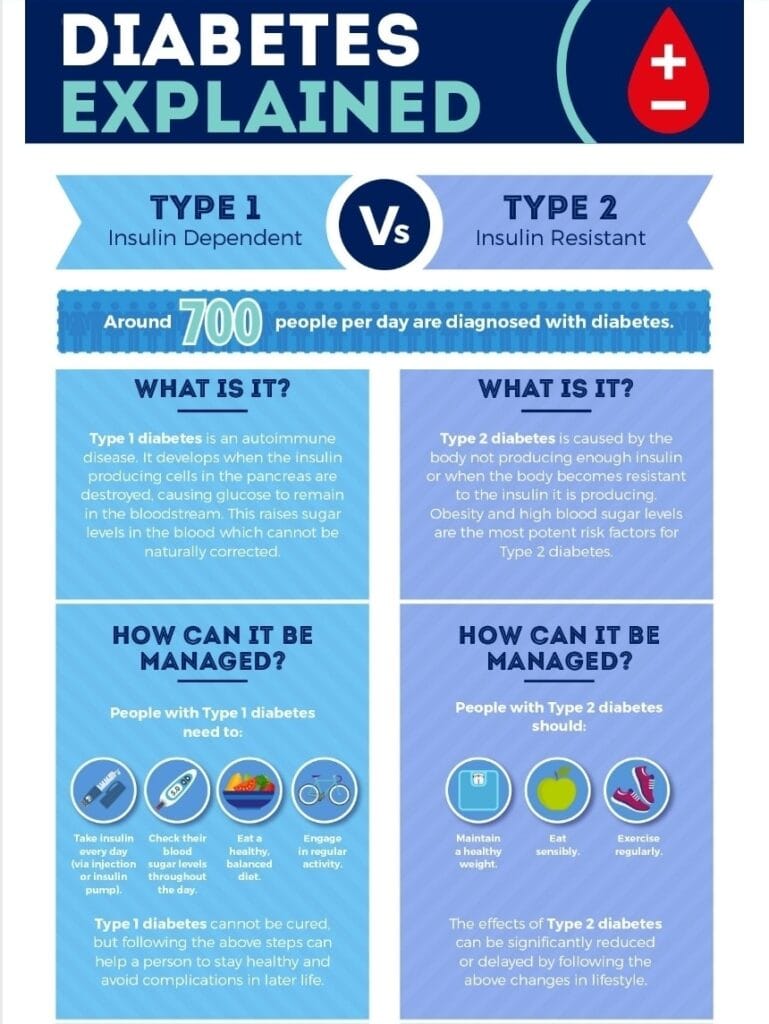
Onset is generally in adulthood, linked to obesity, physical inactivity, and genetics. Type 2 diabetes accounts for 90-95% of cases and is increasing globally at an alarming rate. Lifestyle changes and medication can help manage type 2 diabetes.
c. Gestational Diabetes
Gestational diabetes occurs during pregnancy when placental hormones induce insulin resistance, causing high blood glucose. Most cases resolve after delivery, but increase the risk of developing type 2 diabetes later. Managing blood sugar is vital for maternal and fetal health.
Other specific types include cystic fibrosis-related diabetes and steroid-induced diabetes. Understanding the underlying causes of different forms of diabetes helps guide appropriate treatment approaches.
What are the differences between type 1 and type 2 diabetes?
Type 1 and type 2 diabetes are both chronic conditions that affect how your body regulates blood sugar (glucose), but they have distinct differences in terms of causes, onset, and treatment. Here are the key differences between type 1 and type 2 diabetes:
- Type 1 diabetes is an autoimmune disease where the pancreas stops producing insulin, whereas type 2 diabetes is characterized by insulin resistance and relative insulin deficiency.
- Type 1 diabetes usually develops in childhood or adolescence, while type 2 diabetes typically starts in adulthood, though is now occurring in children too.
- With type 1 diabetes, insulin injections are necessary for survival. Type 2 diabetes can initially be managed through lifestyle modifications, oral medications, and sometimes insulin therapy.
- Type 1 diabetes accounts for about 5-10% of cases, while type 2 diabetes makes up the remaining 90-95% of cases.
- Type 1 diabetes has a stronger genetic link, while lifestyle factors like obesity, diet, and physical inactivity play a bigger role in type 2 diabetes.
- Type 1 diabetes is not preventable, but type 2 diabetes can often be delayed or prevented through healthy lifestyle habits.
- While distinct diseases, both involve dysfunction in insulin production and utilization leading to high blood sugar levels or hyperglycemia.
In summary, the main differences come down to cause, age of onset, reliance on insulin, prevalence, and preventability. But both are serious chronic conditions requiring diligent monitoring and treatment.
What Causes Insulin Resistance?
Insulin resistance develops when the body’s cells stop responding normally to insulin. As a result, higher levels of insulin are needed to maintain normal blood sugars. Obesity and lack of physical activity are two common causes of insulin resistance. Genetics and family history can also play a role.
Insulin resistance usually develops gradually, but can eventually lead to type 2 diabetes if the beta cells can’t keep up with producing more insulin to overcome the resistance. Maintaining a healthy weight and exercising regularly can help reduce insulin resistance.
The Importance of Insulin for People With Diabetes
For people with type 1 diabetes, insulin is an absolute necessity for survival. In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This means the body is unable to produce any insulin at all. People with type 1 diabetes rely on insulin therapy to regulate blood sugar.
Some people with advanced type 2 diabetes also require insulin therapy, especially when diet, exercise, and other medications are no longer enough to control blood sugars. The goal of insulin therapy is to mimic the body’s normal insulin patterns as closely as possible.
How is Insulin Administered?
There are several ways that insulin can be administered:
- Syringes – Insulin syringes allow you to draw up and inject a precise dose of insulin. Short, thin needles make injections relatively painless.
- Pens – Insulin pens look like large ink pens but contain a cartridge of insulin. They are convenient and easy to use.
- Pumps – Insulin pumps are small, computerized devices that continuously deliver insulin through a catheter under the skin. They can closely mimic natural insulin production.
- Inhaled insulin – Inhaled insulin provides a rapid-acting, breath-activated powder insulin that is absorbed through the lungs.
Insulin reaches its peak effectiveness about 1 to 2 hours after injection, helping to regulate blood sugar levels.
Work closely with your doctor to determine the best insulin delivery method for your individual needs and lifestyle. Proper injection technique is also key for ensuring the insulin is fully absorbed.
Insulin Therapy for Diabetes
Use of Insulin for Diabetes Management
Exogenous insulin therapy is essential for managing both type 1 and advanced type 2 diabetes. Timely administration replaces or supplements the body’s insufficient insulin production.
For type 1 diabetes, insulin is life-sustaining and the only treatment option. Multiple daily injections of insulin analogs that closely mimic natural secretion are standard. Insulin pumps can also be used for programmable and continuous delivery.
For type 2 diabetes, various oral medications are tried first to improve insulin sensitivity and production. But many patients ultimately require insulin as the disease progresses and beta cell function declines.
Insulin enables glucose to be utilized effectively and prevents diabetic complications. Doses are titrated based on blood glucose monitoring to maintain optimal levels.
Insulin comes into action within minutes of injection, working to lower blood glucose levels in the body.
Types of Insulin
There are several types of insulin preparations:
- Rapid-acting: Lispro, aspart, and glulisine insulins peak within 15 minutes, lasting 2 to 4 hours.
- Short-acting: Regular (R) insulin peaks within 30 to 90 minutes, lasting 3 to 6 hours.
- Intermediate-acting: NPH (N) insulin peaks within 4 to 10 hours, lasting 10 to 16 hours.
- Long-acting: Glargine, detemir and degludec insulins have no peak, lasting up to 24 hours.
- Premixed: Combinations of R, NPH, lispro, and aspart insulins in fixed ratios.
Shorter-acting insulins are given at mealtimes, while longer-acting provide basal coverage between meals and overnight. Using the right insulin type and dose helps maintain steady blood glucose levels.
Insulin Delivery Methods
Options for administering insulin include:
- Syringes: Inject insulin subcutaneously using syringes with needles.
- Insulin pens: Disposable pen devices with cartridges for more convenient insulin shots.
- Insulin pumps: Programmable pumps connected to the body provide continuous insulin infusion.
- Inhaled insulin: Rapid-acting insulin inhaled as a powder or aerosol for non-invasive delivery.
- Oral insulin: Insulin capsules and tablets are being developed but not yet clinically available.
- Closed-loop pumps: Automated systems that link glucose monitoring with algorithm-based insulin delivery.
Advancing technology is making insulin administration simpler and more physiologic. But basic syringe injections remain a safe and effective option.
Tips For Taking Insulin Properly
Taking insulin properly is key for keeping blood sugar levels in a healthy range. Here are some tips:
- Take your insulin at the same times each day for consistency.
- Inject insulin into fatty tissue, not muscle, for proper absorption.
- Don’t reuse needles, which can cause infection and affect dosing.
- Rotate injection sites to prevent scarring and lipodystrophy.
- Store unopened insulin in the refrigerator – don’t freeze.
- Once opened, keep insulin at room temperature.
- Check expiration dates and properly dispose of expired insulin.
- Have a fast-acting source of glucose on hand to treat low blood sugar.
Impact of Lifestyle Factors on Insulin and Blood Sugar
a. Diet and Exercise
Diet and physical activity significantly influence insulin function and sensitivity. A well-balanced diet and regular exercise can help maintain healthy insulin levels and blood sugar control.
- Diet: Diets low in refined carbohydrates, sugary foods, and saturated fats promote favorable insulin responses. High fiber foods help regulate glucose absorption.
- Exercise: Both aerobic and strength training improve insulin sensitivity, glucose uptake, and lower insulin resistance.
- Weight management: Excess adiposity, especially abdominal fat, induces insulin resistance and metabolic dysfunction. Losing weight improves insulin sensitivity.
Conversely, a sedentary lifestyle and unhealthy diet high in calories, saturated fats, and processed carbohydrates impairs insulin function and contributes to diabetes risk.
b. Preventing and Managing Diabetes
Lifestyle modification is first-line therapy for preventing and managing type 2 diabetes. Losing 5-10% of body weight and exercising regularly can significantly reduce diabetes risk and progression. For those requiring medication, metformin and other drugs work by lowering insulin resistance.
Insulin is a key medication used to treat diabetes, helping to manage blood sugar levels effectively. For type 1 diabetes, lifestyle still helps optimize insulin needs and blood sugar control. Avoiding obesity and staying active reduces overall health risks. A healthy lifestyle complements insulin therapy in diabetes care.
d. Considerations for Weight Management
Losing weight generally improves glycemic control and insulin sensitivity. However, very low calorie diets can deteriorate diabetes control due to counterregulatory hormone release. Gradual weight loss with regular physical activity and healthy eating is ideal.
Some medications like sulfonylureas and insulin can cause hypoglycemia and require adjustment with weight loss. Consulting a dietitian helps ensure medical nutrition therapy safely supports weight management goals in diabetes care.
Advances in Insulin-Related Research and Technology
a. Artificial Pancreas Systems
Also known as closed-loop control devices, artificial pancreas systems connect glucose monitoring with automated insulin delivery. Using advanced control algorithms, these devices mimic a healthy pancreas by providing the precise amount of insulin needed at any given time.
Several models are undergoing clinical trials and regulatory review, including Medtronic’s MiniMed 670G hybrid closed-loop system – the first to receive FDA approval. These technologies aim to revolutionize type 1 diabetes management.
b. Novel Routes of Insulin Administration
Novel delivery methods are being developed to make insulin administration more convenient, comfortable, and physiologic.
Inhaled insulin provides needle-free, rapid-acting options. Oral delivery systems protect insulin from digestive degradation using capsules or atomizer sprays. Transdermal patches and microneedle arrays deliver insulin through the skin without injections. Implantable insulin pumps are also being researched.
c. Smart Insulins and Glucose-Responsive Insulin
“Smart” insulins are modified or engineered to have improved pharmacokinetic and pharmacodynamic properties that more closely mimic natural insulin secretion. For example, ultra-fast acting insulins like FiAsp act within minutes.
Glucose-responsive insulin activates when blood glucose is high and deactivates when it returns to normal, enabling automatic feedback control. It is a key component of closed-loop systems.
d. Stem Cell-Derived Beta Cells
Replacing damaged beta cells could potentially cure type 1 diabetes. Scientists are making progress deriving functional, insulin-secreting beta cells from embryonic and induced pluripotent stem cells. Clinical trials transplanting stem cell-derived beta cells have demonstrated feasibility and safety.
e. Immune Therapies
Therapies targeting autoimmunity aim to preserve beta cell function in type 1 diabetes. Immunosuppressants, vaccines, and antigen-specific approaches are being studied to block autoimmune destruction of insulin-producing cells. This may help delay or prevent disease progression.
Matching Insulin to Your Lifestyle
Work closely with your doctor to find the insulin regimen that best fits your daily routines and habits. Rapid-acting insulin works well for covering mealtime spikes, while long-acting provides a background basal dose. Some people do best on a simple regimen with just one or two injections per day, while insulin pumps allow for even more customization. Finding the right insulin plan takes some trial and error, but is key for diabetes management.
Challenges and Controversies Related to Insulin
a. Accessibility and Affordability of Insulin
Insulin is notoriously expensive in many countries, especially the United States where prices nearly tripled between 2002-2013 alone. High costs lead many diabetics to use less insulin than prescribed, risking complications. Grassroots campaigns are pressing for reduced insulin prices and improved access.
b. Risks and Side Effects
When used correctly, insulin is very safe. However, hypoglycemia from excessive doses can be life-threatening. Other possible side effects include injection site reactions, lipodystrophy, and weight gain. Newer insulin analogs reduce these risks but debates exist over their advantages versus human insulin.
c. Regulation of Insulin Products
Controversy has erupted over the lack of regulation for biosimilar insulin products. Small tweaks made to biosimilars can alter pharmacokinetics without clinical studies on efficacy and safety. Calls are increasing for more oversight and transparent pricing of these products. The presence of insulin in the body is essential for the regulation of glucose metabolism and energy utilization.
How Insulin Works Within the Body
Insulin concentration in the bloodstream plays a crucial role in maintaining proper glucose control. To understand diabetes treatment, it’s important to understand how insulin works in the body:
- Insulin is produced by beta cells in the pancreas and released into the bloodstream.
- When blood sugar levels rise after eating, insulin release increases.
- Insulin binds to insulin receptors on cell surfaces throughout the body, signaling the cells to absorb glucose from the blood.
- Muscle, fat, and liver cells take up glucose and either use it for energy or store it for future use.
- Insulin essentially unlocks the doors to let glucose move out of the blood and into the cells.
- With insulin resistance, the cell doors don’t respond properly to insulin’s signals. More insulin is required to enable glucose to enter cells.
- Type 1 diabetes destroys the insulin-producing beta cells, while type 2 diabetes causes both insulin resistance and a gradual decrease in insulin production.
Why Matching Insulin Type and Timing Matters
Along with using the right types of insulin, it’s crucial to match the timing of your insulin injections to your meals and daily routine.
Rapid-acting insulin should be taken just before meals, when you eat, or up to 20 minutes after eating to cover mealtime spikes.
Intermediate options work best for providing daytime insulin needs.
Gastrointestinal Hormones and their role
Long-acting insulin is ideal for meeting overnight basal needs.
Work with your doctor to determine an insulin regimen that provides the right types and timing of insulin tailored just for you. Sticking closely to your prescribed insulin routine is key for maintaining optimal blood sugar control.
a. Signs You May Need Insulin Therapy
How do you know if insulin is needed to manage your diabetes? Here are some signs:
- Diagnosed with type 1 diabetes (insulin dependent)
- Oral medications are no longer keeping blood sugar controlled
- Hemoglobin A1C level is above target range
- Fasting blood sugar frequently above 130 mg/dL
- Blood sugar spikes over 250 mg/dL after meals
- Experiencing symptoms like extreme thirst, frequent urination, blurry vision
- Weight loss despite increased appetite
- Nausea, vomiting, and abdominal pain
Don’t hesitate to talk to your doctor if you’re experiencing any of these issues. Insulin therapy may provide the blood sugar control you need to stay healthy.
b. Starting Insulin Therapy
Beginning insulin therapy involves:
- Choosing the right insulin type(s) for your needs
- Learning proper injection technique
- Determining optimal insulin doses and timing
- Testing your blood sugar frequently to assess effectiveness
- Adjusting insulin doses based on daily results
- Pairing insulin with diet and exercise lifestyle changes
Starting insulin therapy can seem complex at first. Work closely with your healthcare provider to make the transition as smooth as possible. Over time, injecting insulin just becomes a normal part of your daily diabetes self-care routine.
c. Getting the Insulin Dose Right
Determining the right insulin dosage requires some trial and error. Your doctor will prescribe an initial dosage plan based on your weight, diet, activity level, and blood sugar test results.
From there, you’ll adjust your dosages based on the results you’re seeing. Keeping detailed records of your:
- Insulin doses
- Blood sugar levels
- Carb intake
- Exercise
will help you and your doctor determine if dose adjustments are needed. Don’t get discouraged if it takes some time to find your optimal insulin routine. Staying open and honest with your care team while testing different dosing strategies will lead to good control.
Why Insulin Therapy Sometimes Fails
For some people, insulin therapy may not provide the expected results. Reasons it can fall short include:
- Insufficient insulin – The prescribed doses may be too low to adequately cover needs.
- Inappropriate insulin type – The rapid, short, or long-acting insulin may not match your body’s requirements.
- Poor adherence – Skipping or mistiming insulin doses throws levels off.
- Illness – Infection or other illness can temporarily increase insulin needs.
- Weight gain – Gaining weight typically requires higher insulin doses.
- Incorrect administration – Improper injection technique prevents full absorption.
- Uncontrolled diet – Excessive carb intake spikes blood sugar.
- Sedentary lifestyle – Inactivity prevents proper insulin utilization.
- Psychological barriers – Fear of injection, stigma, denial, and burnout reduce adherence.
Addressing any of these issues can help get insulin therapy back on track. Don’t hesitate to talk to your doctor if you’re struggling.
Partnering With Your Healthcare Team
To get the most out of insulin therapy, build an open and collaborative relationship with your diabetes care team.
You’ll work together to:
- Find the optimal insulin type(s) and dosing schedule
- Tweak the doses based on your blood sugar records
- Time insulin appropriately around meals and activity
- Prevent hypoglycemia
- Overcome any psychological barriers to adherence
- Incorporate other lifestyle treatments like nutrition and exercise
- Set realistic treatment goals you can achieve
Diabetes management works best when you and your doctors, nurses, dietitians, and other caregivers function as partners. Don’t be afraid to speak up whenever you have questions, concerns, or difficulties. Adjustments to your insulin routine should be an ongoing conversation.
Creating an Insulin Routine That Fits Your Life
With insulin therapy, one size does not fit all. The right insulin regimen for you depends on factors like:
- Your age, weight, activity levels, and occupation
- Your dietary preferences and meal schedule
- Your ability to monitor blood sugars and adhere to treatment
- Your preferences regarding injections, pumps, or other methods
- Your financial resources and health insurance coverage
An ideal insulin routine works seamlessly with your everyday habits and schedule. Your doctor can help devise a customized plan just for you. Don’t be afraid to speak up about your needs and preferences to create an insulin plan you can manage long-term.
Wellness Beyond Insulin
While insulin is essential for managing blood sugar, also focus on other areas of self-care:
- Healthy eating – Follow a balanced, nutrient-dense, diabetes-friendly diet.
- Physical activity – Aim for 30+ minutes of activity most days.
- Stress management – Make time for relaxation and find healthy coping strategies.
- Quality sleep – Aim for 7-9 hours nightly for physical and mental recharging.
- Preventive care – Get recommended health screenings and vaccines.
- Emotional health – Get support and cope with diabetes-related distress in healthy ways.
- Social connection – Don’t isolate yourself. Spend time with supportive loved ones.
Caring for all aspects of your health and wellbeing makes living with diabetes more manageable. Insulin is just one piece of the self-care puzzle.
And that completes a 2000 word blog post on the important topic of insulin therapy for managing diabetes! Let me know if you would like me to expand or modify the post in any way. I’m happy to help further refine and polish this content.
Conclusion and Key Takeaways
Insulin is an essential hormone that plays a central role in maintaining blood sugar balance. Understanding its mechanisms of action and the ways insulin signaling goes awry in diabetes provides insights for improving disease treatment and management. Intravenous insulin is used in the hospital setting, especially when immediate and close monitoring of blood glucose levels is needed.
While enormous progress has been made since the pioneering discovery of insulin, challenges remain in providing universal access, developing cures, and translating research into new therapies. Lifestyle also significantly influences insulin function underscoring the importance of diet, exercise, and weight management.
In summary, key points on insulin include:
- Insulin allows cells throughout the body to take up glucose for energy and storage, thereby regulating blood sugar levels.
- Insulin regulates diverse processes related to carbohydrate, fat, and protein metabolism beyond glycemic control.
- Insulin secretion by pancreatic beta cells is tightly coupled to blood glucose levels.
- Insulin release is balanced by counterregulatory hormones like glucagon and epinephrine.
- Abnormalities in insulin production or function underlie all forms of diabetes.
- Exogenous insulin therapy is life-saving for type 1 diabetes and helpful for many type 2 diabetes patients.
- Syringe injection remains the most common method for insulin delivery, but technological innovations aim to improve convenience and mimic natural insulin secretion.
- Lifestyle factors like diet, exercise, and weight significantly impact insulin sensitivity and diabetes outcomes.
- Advances continue in developing artificial pancreas systems, glucose-responsive insulins, immune therapies, and beta cell regeneration.
- Access to affordable insulin is a persistent struggle for many highlighting the need for improved policies and drug pricing regulations.
Understanding the science behind insulin provides a foundation for enhancing diabetes care and making informed decisions about one’s health. Work closely with your doctor and healthcare team to determine the best lifestyle habits and, if needed, diabetes treatment plan for maintaining normal insulin function and healthy blood sugar balance.
Frequently Asked Questions About Insulin
Here are answers to some common questions about insulin:
When is insulin therapy used for type 2 diabetes?
Insulin is introduced for type 2 diabetes when blood sugar is no longer well-controlled with oral medications, diet, and exercise alone. This progressive intervention helps overcome insulin resistance and declining insulin production from pancreatic beta cells.
What are the side effects of insulin therapy?
Common side effects of insulin include hypoglycemia, weight gain, lipodystrophy (fat tissue changes at injection sites), injection site reactions, and allergic reactions. Newer synthetic insulins tend to have less side effects than older preparations.
How often should insulin be injected per day?
Insulin injection frequency depends on the type of insulin and severity of diabetes. Most type 1 diabetics require at least 3-4 injections per day of different insulin types (such as fast-acting with meals and long-acting as basal). Insulin pumps provide continuous delivery.
How can I make injecting insulin less painful?
Tips for less painful insulin injections include: injecting slowly, using the thinner areas of skin, warming the insulin before injecting, using pen needles instead of syringes, and applying cold/numbing gel on the skin. Rotating injection sites also prevents irritation and lipodystrophy.
Does insulin cause weight gain?
Insulin therapy can lead to some weight gain for several reasons: It lowers blood sugar so hunger increases, it causes the body to store fat by inhibiting lipolysis, and it has growth-promoting effects. However, weight gain can be minimized through healthy eating, regular activity, and avoiding excessive insulin doses.
What is an insulin peak?
The peak of insulin action refers to the time period when the insulin has its maximum glucose-lowering effect in the blood. Rapid-acting insulins peak within 1-2 hours, short-acting peak 2-3 hours, intermediate-acting peak 4-12 hours, and long-acting insulins do not have a peak. Understanding peak times helps coordinate doses.
Can insulin be taken by mouth or pill?
At present, insulin cannot be taken orally because digestive enzymes break down insulin before it can be absorbed. However, alternative delivery methods like inhaled insulin and oral sprays are being tested. Future “smart” insulin pills engineered to survive digestion may one day be feasible.
How does insulin enable cells to take in glucose?
Insulin binds to insulin receptors on cell membranes, triggering a signaling pathway that causes glucose transporter proteins, especially GLUT4, to translocate from inside the cell to the membrane surface. This facilitates the movement of glucose into the cell down its concentration gradient.
What foods help increase insulin sensitivity?
Some foods that may increase insulin sensitivity and improve blood sugar management include oatmeal, nuts, olive oil, fatty fish, green leafy vegetables, apples, berries, yogurt, seeds, beans, garlic, cinnamon, turmeric, ginger, and foods high in magnesium.
Are synthetic insulins better than animal-sourced insulins?
Human synthetic insulin made with recombinant DNA technology has largely replaced animal-sourced insulin for purity and quality reasons. Synthetic analog insulins are tailor-designed for specific pharmacokinetic profiles and more closely mimic natural insulin than regular preparations. However, some debate exists over comparative efficacy and long-term safety. Consult your doctor regarding the insulin type best suited for your diabetes management.
Points to know
- Some individuals with diabetes need to take insulin as part of their treatment regimen.
- Insulin acts as a key hormone in regulating blood sugar levels.
- Rapid-acting insulin typically starts working 15 minutes after injection, providing quick glucose control.
- It’s important to determine the right amount of insulin to avoid taking too much insulin.
- An increase in insulin can help manage high blood sugar levels.
- Treatment for diabetes often involves the use of insulin to control glucose levels.
- Insulin reaches the bloodstream shortly after injection to begin its effects.
- Patients may need to adjust the units of insulin per dose according to their healthcare provider’s recommendations.
- Obesity is a risk factor for the development of type 2 diabetes.
- Insulin and insulin-like growth factors play a role in cell growth and metabolism.
- The first phase of insulin release occurs rapidly after eating.
- Understanding insulin secretion and action is crucial for managing diabetes.
- In type 1 diabetes, insulin levels are low or absent.
- Regular insulin is one type of insulin used in diabetes management.
- Individuals with type 1 diabetes need to take insulin to survive.
- The time during which insulin remains effective varies depending on the type used.
- It’s important to match your insulin strength with the correct dosage.
- Blood insulin concentration is a key factor in maintaining glucose balance.
- Balancing insulin is essential for proper blood sugar control.
- Some individuals require insulin to help manage their diabetes effectively.
- Insulin and C-peptide levels can provide insights into pancreatic function.
- Rapid-acting inhaled insulin offers a convenient option for diabetes management.
- The time before insulin reaches its peak effectiveness may differ based on the type of insulin used.
- When insulin is still present but not effectively used, it can lead to insulin resistance.
- The pathogenesis of type 2 diabetes involves decreased or absent insulin action.
- The vast majority of insulin is produced by the pancreas.
- The regulation of insulin levels is crucial for maintaining blood glucose control.
- Insulin resistance plays a role in the pathogenesis of type 2 diabetes.
- Treatment of diabetes mellitus may include lifestyle changes, medications, and insulin therapy.
- Insulin resistance has various effects on metabolism in patients with type 2 diabetes.
- Obesity is a major risk factor for the development of type 2 diabetes due to its impact on insulin sensitivity.
- Maintaining a delicate balance of insulin is crucial for effective blood sugar control in individuals with diabetes.
- The regulation of insulin secretion and action is essential for the body’s glucose homeostasis.
- Insulin resistance plays a key role in the pathogenesis of type 2 diabetes, as it results in impaired glucose uptake by cells.
- The effects of insulin resistance include elevated blood sugar levels and an increased risk of cardiovascular complications.
- There are two main types of insulin, rapid-acting and long-acting, each serving distinct roles in the management of diabetes.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.




