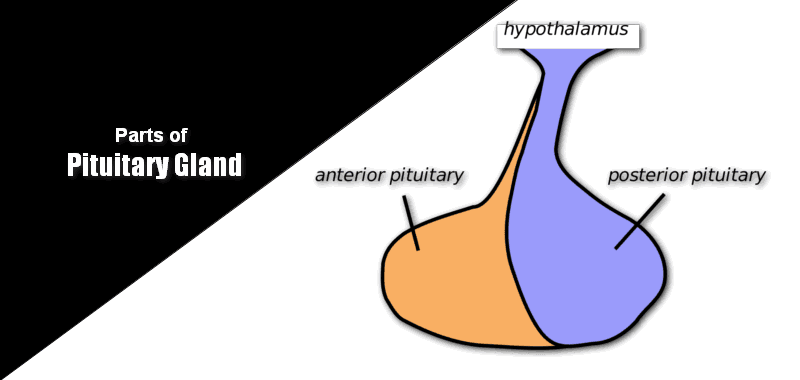
The human pituitary gland is a reddish-gray structure about 10 mm in diameter in the brain just behind the optic chiasma as an extension of the field of the hypothalamus. The average weight of the gland in females is 0.5–0.6gm and in males, it is 0.6 to 0.7 gm. The pituitary gland is located below the hypothalamus of the brain.

What are the basic parts of Pituitary Gland?
The pituitary gland is made up of 3 lobes, namely,
- Anterior pituitary gland lobe (70%)
- Pituitary gland Middle lobe (5%)
- Posterior pituitary gland lobe (25%)
| Anterior Pituitary Gland Lobe (70%) | Middle Lobe (5%) | Posterior Pituitary Gland lobe (25%) |
|
|
|
Anterior Pituitary gland lobe
“Andreas Vesalius” described the pituitary body in 1543. The anterior pituitary hormones are tropic (trophikosG =nourishing) or tropins (troposG =turning) in nature, stimulating the secretion of all these hormones from target organs. Hormones secreted by the anterior pituitary are,
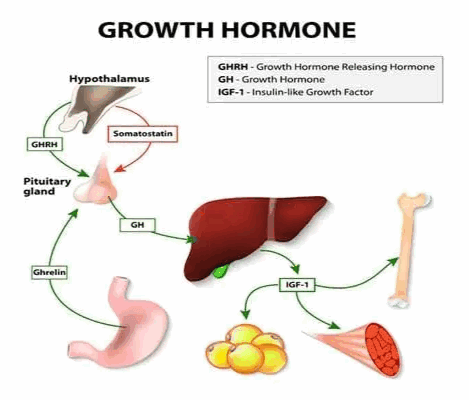
1. Growth Hormone (GH)
Chemistry:
- GH is a single polypeptide, with a molecular weight of about 22,000 in all mammalian species.
- GH is synthesized in “Somatotropes,” a subclass of the most abundant cells in the gland.
- It consists of 191 amino acids.
Functions:
- GH stimulates overall protein synthesis with associated retention of phosphorous, probably by increasing tubular reabsorption.
- GH increases DNA and RNA synthesis.
- It increases the synthesis of collagen.
- GH brings about “lipolysis” in a mild way by mobilizing fatty acids from adipose tissue by activating the hormone-sensitive “triacylglycerol lipase.”
- Hypersecretion of GH can cause hyperglycemia, poor sugar tolerance, and glycosuria.
Abnormality:
- Panhypopituitarism: it is because of decreased secretion of all the anterior pituitary gland hormones. It may be congenital, or it may occur suddenly during the life of the individual.
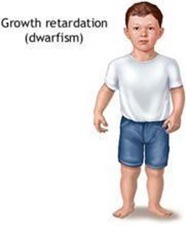
- Dwarfism: It is a result of a deficiency in anterior pituitary gland secretion during childhood.

- Levi-Lorain dwarfism: It is because of a hereditary inability to form somatomedin C, but the rate of GH secretion.
- Acromegaly: It is because of the increased secretion of GH.
For more details:
Kids and teens grow and go through puberty at different times. For girls, puberty usually begins between the ages of 8 and 13. For guys, it often begins later-between 10 and 15. You must have noticed some teens develop a lot earlier, whereas others develop much later than other people of the same age. There’s a medical reason some people grow more slowly than usual.
Reasons for slow growth:
- Genetic Reason: If you’re short, you may just have familial (genetic) short stature. Like short parents, having short children.
- Lack of Nutrition: Not getting adequate amounts of protein, calories, and other nutrients in your diet can also cause growth to slow, and some other chronic medical conditions such as kidney, heart, lung, and intestinal diseases.
- Sickle cell anemia: People with sickle cell anemia may also grow and develop more slowly. Sickle cell anemia is a blood disorder that affects hemoglobin, the protein found in red blood cells (RBC) that helps carry oxygen throughout the body. It occurs when a person inherits two abnormal genes (one from each parent) that cause their RBC to change shape.
- Constitutional growth delay: These teens grow at an average rate when they are younger kids, but they lag and don’t start their pubertal development and growth spurt until after most of their peers.
- Dwarfism results from abnormal growth of the bones and cartilage in the body. In many forms of dwarfism, the person has abnormal body proportions, such as noticeably short limbs.
- Hormones: Many diseases of the endocrine system can impact the growth of the glands that produce hormones. The endocrine glands secrete hormones that are carried throughout the body in the bloodstream. The hypothalamus (part of the brain) controls the pituitary gland, which releases some hormones that regulate growth and sexual development. Estrogen and testosterone are essential hormones that drive sexual development and function and also play a role in growth.
- Hypothyroidism: This can cause slow growth because the thyroid gland isn’t producing enough thyroid hormone responsible for proper growth.
- Turner syndrome: This is a genetic condition (because of a problem with a person’s genes) that occurs in girls. A missing or abnormal X chromosome causes it. Girls with Turner syndrome are short and rarely undergo normal sexual development because their ovaries don’t mature and function normally.
- Growth Hormone Deficiency (GHD): One growth disorder specific to the hormones that govern growth is called growth hormone deficiency. This condition involves the pituitary gland, the small gland at the base of the brain that produces growth hormone and other hormones. If the pituitary gland doesn’t produce enough hormones for healthy growth, growth slows down or stops.
Essential Facts of Growth Hormone Deficiency:
- It can occur at any age.
- The most common sign in kids and teens is a slowing of growth to less than 2 inches (5 centimeters) a year.
- Kids with this disorder usually have normal body proportions.
- Growth hormone deficiency does not affect intelligence or brain function.
- Growth hormone deficiency typically impacts only one person in a family and isn’t passed on from parents to children.
Causes:
In most cases, though, the cause of growth hormone deficiency is merely unexplained.
- Underdeveloped, damaged, or malfunctioning pituitary gland.
- Hypothalamus: This can happen before or during birth or can be caused later by an accident or trauma or certain diseases.
- Tumors near the pituitary gland, like craniopharyngioma, can also damage the hypothalamus and pituitary gland and affect growth.
Symptoms:
- Growth in Height: Affected children have an abnormally slow growth rate.
- Head: Head circumference increases typically in GHD.
- Adiposity: Because of the deficient breakdown of fats, patients have a much higher level of adipose tissue than average for their age, especially around the waist.
- Muscle: Because of reduced protein synthesis, lean body mass, reflected mainly in muscle development, is correspondingly lower than average for age.
- Genitals: Males are underdeveloped for their age, even when gonadotropin secretion is apparently normal.
- Blood Sugar Levels: Because of the inadequate breakdown of glycogen into glucose, hypoglycemia can occur, and seizures may arise if this is severe and untreated.
- Phenotypic Appearance: The above signs and symptoms lead to a “typical” phenotypic appearance for the GHD patient. Thus, and short stature, patients, have a chubby presence, and usually a high-pitched voice. They may seem precocious because their appearance suggests a younger child but their speech and abilities are that of an older child.
Treatment:
- Self Care: As growth hormone deficiency can cause a lack of energy and strength, patients should eat a balanced diet, get regular exercise, and get plenty of sleep.
- Medications: The doctor may prescribe growth hormone, also called somatropin (Humatrope, Genotropin). The drug is given as a shot a few times a week that is injected underneath the fat of the patient’s skin.
- Hormone Therapy: Children and some adults with growth hormone deficiency will benefit from growth hormone therapy. The goals of treatment are to increase growth in children and restore energy, metabolism, and body composition.
Tips for the parents:
- Treat your child according to age, not size. Also, inform their teacher about the correct age.
- Encourage your child to take part in physical activities he or she enjoys.
- Increase your child’s comfort at home by making sure that essential items are within reach, such as the radio, television, stereo, and books.
- Get professional counseling for yourself and your child.
- Self-esteem reflects perceptions or feelings about oneself. Teasing and bullying can have an adverse effect on any child’s self-esteem. Keep the lines of communication open. Encourage your child to discuss any situations or circumstances that may trouble him or her.
It can be tough having a growth disorder as a teen because it can affect a person’s body image and self-esteem. Talking with a mental health professional is one way some people deal with feelings and concerns about their growth.
2. Adrenocorticotrophic hormone (ACTH)
Chemistry:
- It is a straight chain polypeptide with a molecular weight of about 4,500.
- It comprises 39 amino acids residues in mammals like a man, ox, sheep & Pig.
- The most potent segment of activity is from residue 15 to 18.
Functions:
- ACTH increases the synthesis of corticosteroids by the adrenal cortex and also stimulates their release from the gland.
- ACTH is found to increase the transfer of cholesterol from plasma lipoproteins into the fasciculata cells.
- The ACTH induces a rise in cAMP, brings about phosphoryl and activation of “Cholesteryl esterase.”
- the enzyme action ultimately creates a large pool of free cholesterol.
- It activates the rate-limiting enzyme for the conversion of cholesterol to pregnenolone (cholesterol desmolase).
- It activates the dehydrogenases of HMP to increase the concentration of NADPH required for hydroxylation.
- It activates “hormone-sensitive lipase,” which is involved in lipolysis, which increases the level of free fatty acids.
Normal level:
The circulating concentration of ACTH in normal is 0.1 to 2.0 m µ/dl. The pituitary secreter stores 5 to 10mg.
Abnormality (or) Clinical importance:
Cushing’s disease:
- Oversecretion of ACTH leads to Cushing’s disease, because of tumor (or) hyperplasia of β-cells of the anterior pituitary gland lobe.
- It leads to hypersecretion of corticosteroids, especially glucocorticoids.
- It produces symptoms like hyperglycemia, glycosuria, muscle wasting, atrophy of the skin, and high urinary negative nitrogen balance.
- abnormal retention of fats giving a moon-shaped face appearance, retention of sodium ions in water and hypertension.
3. Leutinizing Hormone
Chemistry:
- LH is a glycoprotein in nature; it contains sialic acid, hexose, and hexosamine as the carbohydrate moiety (16%).
- The molecular weight of LH is 40,000.
- LH is a dimer in nature; it consists of α-chain and β-chains linked non-covalently.
- The β-chain of human FSH and LH has 112 amino acid residues.
Functions:
This hormone is also known as “Interstitial Cells Stimulating Hormone (ICSH).” In females,
- It causes the final maturation of graffian follicles and stimulates ovulation.
- It stimulates the secretion of estrogen by the THECA and Granulosa cells.
- It helps in the formation and development of corpus lutem for the luteinization of cells.
- In the ovary, it can stimulate the non-germinal elements, which contain the interstitial cells, to produce androgens, androstenedione, DHEA, and testosterone.
4. Follicle Stimulating Hormone (FSH)
Chemistry:
- The molecular weight of FSH is 25,000.
- These are dimers of α-chain and β-chains linked non-covalently.
- α-Chain is identical to LH and TSH, but the β-chain of human FSH has 118 amino acid residues.
- Glycoprotein in nature, with sialic acid, hexose, and hexosamine as the carbohydrate moiety (16%).
Functions:
It brings about its action through a specific receptor binding and cAMP.
In Females,
- It promotes follicular growth.
- It prepares the graffian follicle for the action of LH.
- Furthermore, it enhances the release of estrogen induced by LH.
In Males,
- It stimulates seminal tubular and testicular growth.
- It plays an important role in the maturation of spermatozoa.
5. Thyroid-Stimulating Hormone (TSH)
Chemistry:
- It is a glycoprotein with a molecular weight of 30,000.
- Each molecule has 8 to 9 cysteine residues.
- It is produced by “basophil cells” of the anterior pituitary organ lobe.
- It consists of α-chain and β-chains linked non-covalently. • The α-chain subunit of TSH, LH, HCG, and FSH is nearly identical.
- The α-subunit consists of 92 amino acids and the -subunit consists of 112 amino acids.
Functions:
It stimulates the activity of the thyroid gland and enhances the rate of specific reactions, such as
- The thyroid gland removes iodine from the blood.
- Conversion of iodide to thyroid hormones.
- The release of hormonal iodide from the thyroid.
Middle Lobe
Melanocyte-stimulating Hormone (MSH)
The hormones secreted by the intermediate lobe (or) middle lobe of the pituitary gland are called “MSH.”
- POMC (Proopiomelanocortin) is the precursor molecule, which is cleaved by “Proteases” to give ACTH, and β-MSH is familiar to both α-MSH and ACTH.
- The ACTH further cleaved to β-MSH, which has 13 amino acids.
- It also α-MSH which is present in more significant quantities.
- Amino acids 11 to 17 of β-MSH are common to both α-MSH and ACTH.
Functions:
MSH darkens the skin and is involved in skin pigmentation by deposition of mammalian melanocytes.
Abnormality:
Addison’s disease:
- MSH is in excess, which increases the synthesis of melanin, resulting in brown pigmentation of the skin.
- Such a condition occurs in this disease.
Posterior Pituitary Gland Lobe
The posterior pituitary secretory lobe contains two hormones.
1) Vasopressin
2) Oxytocin (or) Ocytocin
1. Vasopressin
- It is also called “Arginine Vasopressin”(AVP).
- If “Arg” is replaced by “Lysine,” it is called “Lysine vasopressin” (LVP).
- It is “Nonapeptide,” it consists of nine amino acids.
Mechanism of Action:
ADH binds to membrane receptors and activates adenyl cyclase. The cAMP thus produced will activate the protein kinase. In turn, it phosphorylates proteins in the microtubules and microfilaments. The net effect is the reabsorption of water.
Functions:
a) Antidiuresis:
Vasopressin causes “Antidiuresis.” It increases the permeability of the collecting ducts and tubules to water and allows most of the water to be reabsorbed as the tubular fluid passes through these ducts, thereby conserving water in the body and producing very concentrated urine.
b) Urea-retention effect:
Vasopressin increases the permeability of the medullary collecting dust to urea. I lead to the retention of urea and subsequently contributes to hypertonicity of the medullary interstitium.
c) Pressor effect: It stimulates the contraction of smooth muscles and thus causes vasoconstriction by increasing cytosolic Ca +2 contraction.
e) Glycogenolytic effect: By increasing, intracellular Ca +2 concentration, causes glycogenolysis.
Abnormality:
Deficiency of ADH leads to “Diabetes insipidus,” it is characterized by the excretion of large volumes of dilute urine. Excess secretion of ADH often results from the ectopic production of ADH by malignant tumours, referred to as the “Syndrome of Inappropriate Secretion of ADH” (SIADH). There is the hypotonic expansion of extracellular volume, with hyponatremia.
2. Oxytocin (or) Ocytocin
The term means (Ocy G=quick; tokos G=birth) “to stimulate birth.” It is a polypeptide, each containing nine amino acids, so it is called the Nona peptide.
Mechanism of action:
Oxytocin acts on an estrogen-primed uterus. When uterine labor is near, the numbers of oxytocin receptors are increased by 100 to 200 times.
Function:
Oxytocin mainly causes smooth muscle contraction.
- Effect on the uterus and birth: Oxytocin causes the contraction of the pregnant uterus, especially toward the end of gestation, and is partially responsible for affecting delivery.
- Effect of oxytocin on milk ejection: Oxytocin impacts the mammary gland. Suckling generates a neurogenic reflex that stimulates the production of oxytocin. It causes contraction of the myoepithelial called expelling the milk into milk ducts from the acini.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.