- Adrenal gland locates on the topside of the kidney.
- In human, two adrenals are present on each kidney.
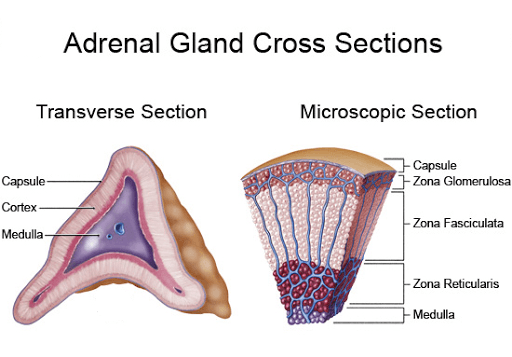
- Histologically, the adrenal has two distinct parts namely,
- An outer covering called the “Cortex”
- surrounding by an inner dark-colored mass called the “Medulla”.
Adrenal Cortex:
The adrenal cortex is made up of three layers,
- Zona Glomerulosa: Outer narrow layer, it is the site of biosynthesis of the “Mineralocorticoid hormones”.
- Zona Fasciculata: Middle layer, site of the production of “Glucocorticoid hormones” and “Adrenal androgens”
- Zona reticularis: Inner narrow layer, secreting “Glucocticoids” along with the middle zone.
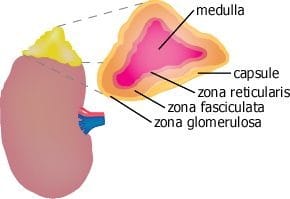
Adrenal medulla:
Adrenal medulla is the inner most part of the gland, which is dark-colored mass. It secretes two distinct hormones, namely;
- Epinephrine (or) Adrenalin
- Norepinephrin (or) Noradrenalin
Adrenal Cortex Hormones:
Glucocoticoids:
- Glucocoticoids are an essential component of adaptation to “Severe stress”
- The cortex has THREE distinct layers in the given figure
- The most important of which is to promote “Gluconeogenesis”.
- Glucocorticoids are 21Carbon steroids, with many actions.
- Glucocoticoids are
a) Cortisol –> Predominant Glucocorticoids in humans, is made in the zona fasiculata.
b) Corticosterone –> less available in humans.
Synthesis:
Cortisol synthesis requires three hydroxylases that act sequentially on the C17, C21, C11 positions. Cortisol circulates in plasma in protein bound and free form. The main plasma bounding protein is an ”a-globulin” called ”Corticosteroid Binding Globulin”(CBG).
Secretion:
The secretion of cortisol is dependent on ACTH which in turn regulated by “Corticotropic releasing Hormone”.
Functions:
A) Effects on intermediary Metabolism:
- Increase glucose production in liver by increasing the delivery of amino acids (Gluconeogenic substrae) from peripheral tissues.
- Promote protein and RNA metabolism.
- Promote lipolysis but can cause lipogenesis on other sides (Face and trunk) especially higher than physiological levels.
B) Effect on host defense:
- Suppress the immune response by decreasing the number of circulating Glucosides and the migration of tissue leucocytes.
- Necessry for maintanance of BP and cardiac output disorders of glucocoticoid hormones.
Addision’s disease: Primary adrenal insufficiency results in hyperglycemia, extreme sensitivity to insulin, intolerance to stress weighloss, nausea, patients with addision’s disease have low BP.
Cushing’s syndrome: Glucocorticoid excess commonly called Cushing’s syndrome is usually due to pharmacologic use of steroids but may result from an ACTH secreting pituitary adenoma.
Mineralocorticoids:
Mineralocorticoids occur in Zona-glomerulosa. Mineralocorticoids are also 21 carbon steroids. Aldosterone is the most potent hormone in this class.
Synthesis:
Synthesis occurs in zona glomerulosa. For the formation of aldosterone from progesterone are 2 smooth endoplasmic reticulum enzymes. 3 -b-hydroxy steroid dehydrogenase and D5, 4-Isomerasee.
Secretion:
Aldosterone is the most potent mineralocorticoid does not have any specific plasma transport protein. But it forms a very weak association with albumin.
Regulation:
Aldosterone regulated by Renin, angiotensin system. This system is involved in the regulation of BP and electrolyte metabolism. Renin is an enzyme produced in the renal afferent arteriole.
Effect:
The primary action of these hormones is to promote retention of Na+ and excretion of K+ and H+ in the renal tubule. ATP provides the energy for this active process. Aldosterone increases the number of membrane sodium channels. Aldosterone produces in response to change in the plasma levels of K and angiotensin-II. Aldosterone increases the activity of several mitochondrial enzymes.
Pathophysiology:
Conn’s Syndrome: Small adenoma’s of the glomerulosa cells results in primary aldosteronism called Conn’s syndrome. Hypertnsion, Hypokalemia (low levels of K), hypernatremia and Alkalosis. (Adenoma’s – Over production of Aldosterone).
Adrenal Medullary Hormones:
In humans adrenal medulla contains 80% of epinephrine & 20 % nor epinehrine. (“Nor” means-The word “nor” in norepinephrine ( or noradrenaline) was originally coined to indicate nitrogen (N) without (O-Ohne) a radical (R), in this case a methyl group. Epinephrine also called adrenaline. Nor-epinephrine called nor-adrenaline. The above two hormones are called Catacholamine and are closely related to Tyrosine and synthesized in the body from Tyrosine.
Epinephrine differs from tyrosine in following respects.
- It contains additional phenolic group in Meta position to benzene ring.
- Contains hydroxyl group attached to b carbon of the side chain. It has a methyl group attached to amino group.
Nor epinephrine is primarily synthesized in sympathetic nervous system and acts locally as a neurotransmitter at the postsynaptic cell.
Release: The release of catacholamine from the cells of the adrenal medulla is brought about by the action of acetyl-choline released by stimulation of the nerve.
Transport: Epinephrine is bound to plasma proteins mainly to albumin and nor-epinephrine is to a lesser extent.
Mechanism of action: Catacholamine act through cyclic AMP by activating cyclase enzyme present in membrane. CAMP activates protein kinases, which phosphory;ates specific protein.
Adrenaline:
Adrenaline is also known as epinephrine in the US and worldwide, a chemical neurotransmitter (4-[1-hydroxy-2-(methylamino)-ethyl]-1,2-benzenediol) and hormone produced in the adrenal medulla. Adrenalin (without the e) is actually a trade name originally registered to Parke-Davis and Company but the name is in wide-spread use. It is an sympathomimetic amine which causes bronchodilation, vasoconstriction, CNS stimulation and mydriasis. Adrenaline has been used to stimulate the heart in cardiac failure and its actions are mediated by adrenoceptors. Adrenaline was first isolated and identified by John Abel in 1897. Adrenaline biosynthesis is outlined below.
Action:
1) Physiological actions:
- Epinephrine lowers the diastolic pressure. Nor-epinephrine increase both systolic and diastolic blood pressure.
- Epinephrine relaxes the smooth muscles of GIT (Gastro Intestinal Tract)
2) Metabolic effects:
- Epinephrine stimulates glycogenolysis – producing Hyperglycemia.
- In muscle epinephrine also causes breakdown of glycogen by increasing cAMP level.
- Both epinephrine and nor-epinephrine increases breakdown of triglycerides in adipose issue by increasing cyclic AMP level.
- Epinephrine increases hepatic Gluconeogenesis.
- Epinephrine increases blood lactic acid level by promoting muscle glycolysis.
- Epinephrine has a direction inhibitory action on insulin release from beta-cells of pancreas.
Discover more from Biochemistry Den
Subscribe to get the latest posts sent to your email.






